Wastewater can track viruses like Covid-19 — can it do the same for superbugs?
A pandemic program could help reveal the true threat of antibiotic resistance to public health.
Mondays are manhole days for Sean Norman. Along with a team of strong-stomached students, Norman packs his pickup truck with 12 vacuum-sized devices and other gear and heads out across the University of South Carolina campus in downtown Columbia, stopping at the manholes.
As they go, they lower their equipment into the sewers and leave it there. The next day, they haul up the collected wastewater. To preserve Norman’s lab, they hose the sewage-filled tanks down in the back of the truck.
Back at the lab, the liters of raw sewage go into juice blenders to smooth out any solids. Then, finally, the scientists can begin the hard work of discovering what dangers lurk in our waste.
This is a snapshot of Norman’s weekly routine, the culmination of a course he has steered for years as part of an effort to monitor wastewater for disease and dangerous pathogens. And in 2020, while the rest of the world was in various stages of lockdown, Norman joined the ranks of researchers everywhere trying to track, treat, and prevent Covid-19 using the tools he knew best. Wastewater testing is a quick and reliable way to track the levels of Covid-19 in a community since infected people shed the virus in their stool even if they aren’t showing symptoms.
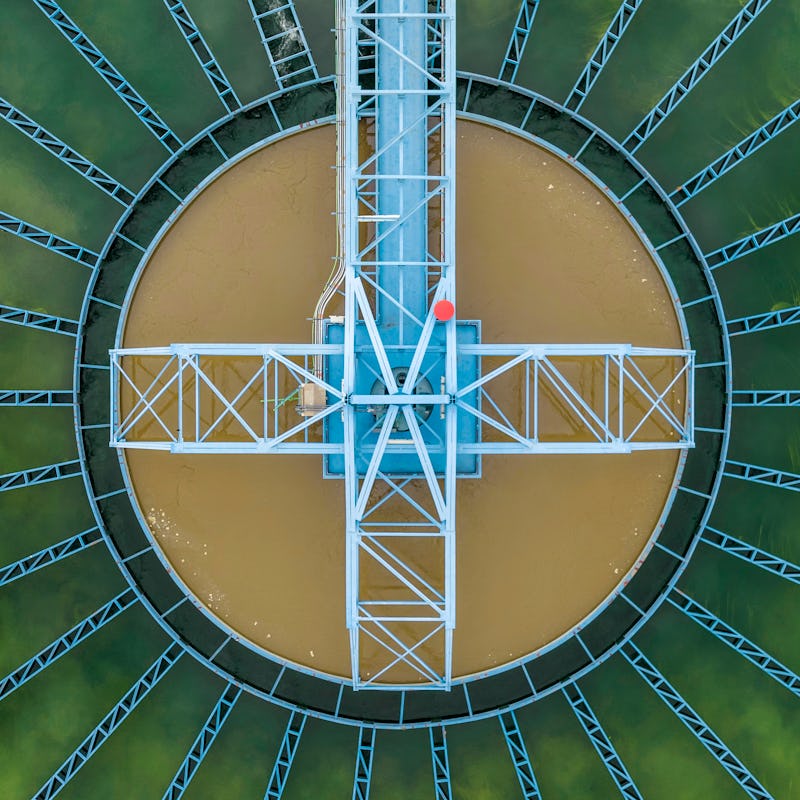
Students working in Norman’s lab retrieve a full sewage sample.
“I am in a school of public health, so my first thing is service to the public,” Norman tells Inverse. In the early part of 2020, his lab pulled regular 15-hour days to kickstart its Covid-19 wastewater testing system. Within a month of lockdown, they tested sewage from a quarter of South Carolina’s residents twice a week. They bought more blenders.
Now, Norman is getting back to his first focus: antibiotic-resistant bacteria. In 2018, Norman’s lab partnered with the U.S. Centers for Disease Control and Prevention to scour sewage for the dangerous microbes impervious to the drugs we rely on to kill them — like methicillin-resistant Staphylococcus aureus (MRSA) or multi-drug-resistant tuberculosis. These bacteria are growing threats to global public health. In the first year of the pandemic, resistant bacteria and fungi killed more than 29,400 people in the United States. Norman himself nearly died from an antibiotic-resistant infection as a child.
The CDC’s National Wastewater Surveillance System (NWSS), created in September 2020 to monitor Covid-19, is expanding to track other disease-causing microbes. By early 2023, the network will test for the most concerning types of antibiotic resistance, influenza, norovirus, Candida auris, SARS-CoV-2, and monkeypox.
“You can find anything you want to find in wastewater.”
It’s a “full circle” moment for the CDC program, which used antibiotic resistance data from the Norman Laboratory to get off the ground when the pandemic hit, says Amy Kirby. Kirby is the program lead for the NWSS at the CDC. The move can’t come a moment too soon: The antibiotic resistance crisis is flourishing in the shadow of Covid-19.
More hospitalizations meant more opportunities for deadly bacteria to evolve and spread since they often thrive in health care settings. Prescribing more antibiotics only worsens the problem — and 80 percent of those hospitalized due to Covid-19 received antibiotics in the first half-year of the pandemic, according to a special CDC report released in July 2022. Infections with antibiotic-resistant bacteria increased by 15 percent during the first year of the pandemic.
These numbers are also incomplete. Covid-19 testing overwhelmed labs that normally test for antibiotic resistance, and people with minor infections were less likely to go to the doctor for testing during lockdown. As a result, nine of the 18 most concerning pathogens are missing key data. Now that the threat of Covid-19 is lessening, it is time to turn wastewater monitoring’s attention back to other dangers to our health and well-being.
“Everybody that’s infected, whether they’re sick or not, they’re going to be shedding those [antibiotic resistant] pathogens in their stool,” Kirby says. “It’s a really good picture of the total antibiotic resistance in a community.”
Norman ran out to a local store and bought kitchen blenders for their “sewage smoothies” — the lab-grade blenders just weren’t enough.
An evolving enemy
Sewage testing has been used across the world for decades to track poliovirus — a pathogen once again making headlines since it was detected in London wastewater and more recently in New York. Local health departments have also used wastewater testing to chart illicit drug usage in their communities.
But for decades, the potential benefits of a national wastewater monitoring network didn’t outweigh the upfront costs.
“Then Covid came along and really changed that calculus and made the investment in building the system worthwhile,” Kirby says.
Now, the NWSS receives data on the levels of SARS-CoV-2 in wastewater from 37 states, four cities, and two territories — but only a dozen states submit their data regularly, according to a related report by POLITICO dating from March (Inverse asked the CDC to confirm this but did not receive a response before publication). Wastewater treatment plants, which already take sewage samples for routine monitoring, send portions to nearby public health labs for testing.
Now that this infrastructure exists for Covid-19, it can be expanded to other viruses, bacteria, and fungi relatively easily, Kirby says. When Inverse asked the CDC if it was ready to expand the program from tracking SARS-CoV-2 to other pathogens, a CDC spokesperson responded:
“Since launching in 2020, NWSS has been shaping independent local efforts into a robust, sustainable national surveillance system. CDC experts are providing ongoing technical guidance and data analysis to participating jurisdictions. We continue to collaborate with implementing partners to develop wastewater surveillance coordination, epidemiology, and laboratory capacity.”
Beyond the infrastructure needed to expand the program, the two years’ worth of incomplete data on antibiotic-resistant bacteria means researchers are starting from a less than ideal base — public health officials don’t know how bad the problem is because no one could devote attention to it.
“There’s more silent infections that we don’t know about.”
Edwin Oh, a geneticist at the University of Nevada, Las Vegas, who began tracking diseases in wastewater when the pandemic began, says missing information is dangerous because public health officials must know exactly what they’re facing to control the resistance crisis.
“Hospitals were just simply swamped,” Oh tells Inverse, recalling the earlier days of the pandemic.
“When you don't have information, this can lead to fear, and fear leads to paralysis,” he adds.
With Covid-19 ebbing, the CDC is directing the wastewater monitors toward other health concerns. Monkeypox testing will begin in the next few months, and antibiotic resistance, influenza, norovirus, and C. auris testing will follow in early 2023.
Inverse asked the CDC to confirm what funding states will receive to support additional wastewater testing and the amount the agency currently spends supporting SARS-CoV-2 testing in the U.S. The agency responded through a spokesperson: “In August 2022, CDC awarded $64 million to support wastewater surveillance capacity in U.S. jurisdictions to detect and track SARS-COV-2.” It did not elaborate on any further funds to support additional testing.
Currently, the CDC is trying to standardize the tests and decide which antibiotic-resistant threats it wants to test for, Kirby says. The agency has not yet decided if it will allow labs to opt out or require the testing. If the effort does span the entire nation, however, the wealth of data collected will be tremendous, experts say.
“You can find anything you want to find in wastewater in terms of antibiotic resistance,” says Tao Yan, an environmental microbiologist at the University of Hawai’i. “That’s the abundance of information there.”
The silent pandemic
Salmonella bacteria can carry some nasty strains of antibiotic resistance.
Yan should know. He has been tracking the spread of illnesses in Honolulu’s wastewater for over a decade. Through his research, he’s found that wastewater testing can catch outbreaks that the health care system misses. He started his wastewater testing program during an outbreak of salmonella in 2010 that sickened at least 21 people in Hawai’i through contaminated fish. As the outbreak petered out, the salmonella strain receded, too.
Then a year later, the same strain of bacteria reappeared in the wastewater. But there were no clinical reports of illness. Most people don’t go to the doctor for diarrhea, after all.
Salmonella outbreaks are always bigger than the official case count, Megin Nichols, an outbreak investigator at the CDC, tells Inverse. For every person who goes to the doctor and tests positive for salmonella, 29 infected people don’t. Nichols is investigating an outbreak of salmonella that has accounted for 884 cases in 48 states, but the incidence is likely upward of 26,000, she says. Of the samples the CDC has taken from the current outbreak, 40 percent show resistance to at least one antibiotic. Fortunately, salmonella is usually not severe and may not require antibiotics, Nichols says.
While less deadly than other diseases, salmonella helps illustrate a problem Kirby calls “silent infections.” Bacteria can infect, mutate, and spread while flying under the clinical radar.
“We need to know, not just fool ourselves.”
That’s where wastewater surveillance comes in. Checking our sewage for bacteria doesn’t depend on people going to the doctor.
As it pivots to antibiotic resistance, the CDC’s National Wastewater Surveillance System won’t test waste for the presence of bacteria but rather for snippets of the DNA that allow bacteria to evade antibiotics, Kirby says.
If the scientists find high levels of a harmful resistance gene, they won’t know if it came from dangerous bacteria or one that doesn’t usually harm humans.
“But in some ways, it doesn’t matter,” Kirby says. Bacteria are promiscuous with their DNA and exchange genes all the time, even between different species. A gene in a harmless bacterium could easily jump to a dangerous one — especially in the literal cesspool of pre-treated wastewater, where all kinds of bacteria mix and mingle.
The national surveillance system will likely focus on resistance genes that protect bacteria from so-called last-resort antibiotics, like carbapenem and colistin, Kirby says.
Physicians could benefit from the real-time resistance information, too.
“I would love to see it be a tool for doctors,” says Amy Pruden, who researches antibiotic resistance in wastewater at Virginia Tech. Doctors could have a better chance of prescribing antibiotics that work if they know what forms of resistance are circulating in the community, she explains to Inverse.
These data could help prevent infections from happening in the first place, too, informing public health policies to stop the spread.
“That’s where the surveillance can help us calibrate,” Pruden says. “Did this intervention or policy change work or make it worse? We need to know, not just fool ourselves.”
Cooperation is key
Antibiotic resistance comes in many forms, so scientists must decide which types to target with testing.
Other countries have already begun testing this wastewater approach. A few international studies have compared the levels of antibiotic resistance in wastewater between countries. And in Finland, a program called WastPan monitors concerning pathogens, including antibiotic-resistant bacteria, to prepare for the next pandemic. The program began in late 2020 and tests the wastewater of 40 percent of Finns.
“We have seen that the wastewater-based surveillance can be very useful and also cost-efficient,” Tarja Pitkänen, who runs the WastPan program at Helsinki University and the Finnish Institute for Health and Welfare, tells Inverse. “From a single sample, you can monitor the whole community.”
Finland’s population is a little larger than South Carolina’s. A national system for wastewater monitoring in the United States would face greater challenges of cooperation. Federal and local health officials, as well as privately-owned laboratories and wastewater treatment plants, must all be on the same page, Pruden says. This has proven challenging throughout the pandemic.
But antibiotic resistance isn’t going away. Bacteria will continue to evolve around the drugs we use to kill them.
“It’s a public health threat that often escapes people’s minds,” Norman says. “People are so used to being able to go to a physician and take a pill to get better.”
Those pills, not even a century old, have secured the health of billions across the globe. To ensure these medications continue to save lives, we need large-scale surveillance systems running in the background that track this silent pandemic as it evolves, Pitkänen says.
“We would be foolish if, once Covid dies down, we just let it go,” microbiologist Yan says.