The Cellular Reset: Inside the Scientific Pursuit of a Universal Cure
Why cure just one disease if you could cure them all?
There comes a point in one’s life — sometimes it’s the big 3-0, sometimes later — when getting old starts to come with some unfortunate side effects. Our joints creak, our muscles ache, and our senses dull.
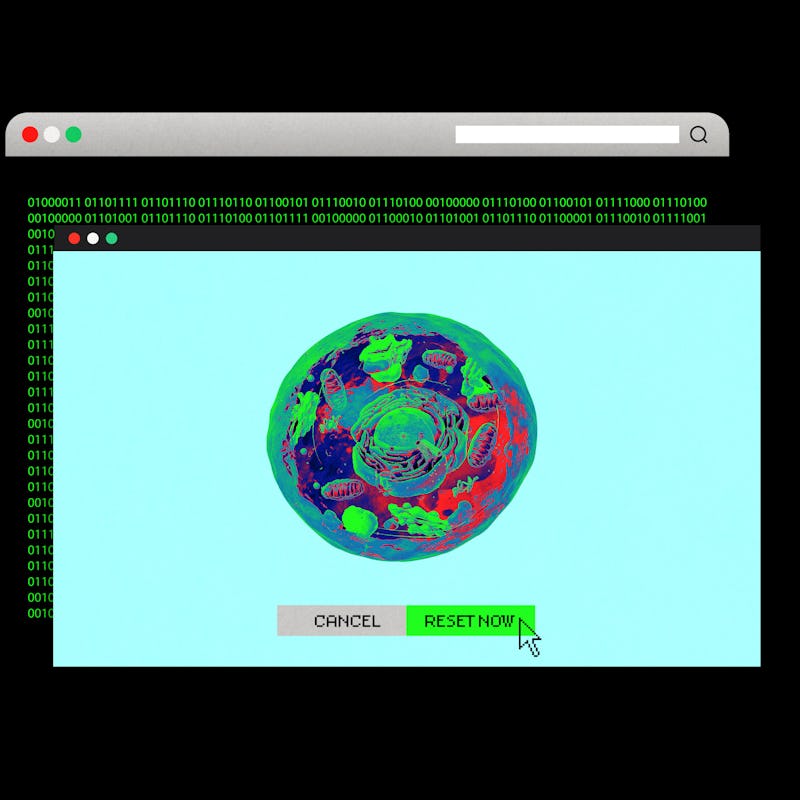
Some people invest in skin fillers or a new training regime to try and spackle over the problem — maintaining the illusion of youthful health, at least for a while. But Wolf Reik is among a small cabal of scientists chasing a Holy Grail of medical innovation that would be a more lasting solution to old age: a biological reset button. Just like the tried-and-true fix for all electronic appliances that go haywire only to come back to full working order after a quick reboot, a reset switch within the body’s basic structure — a cell — might have a similarly restorative and rejuvenating effect. And in 2021, Reik and his team, most notably researcher Diljeet Gill, proved they aren’t chasing some sci-fi fantasy.
In a study eventually published in 2022 in the journal eLife, Gill applied a Nobel Prize-winning technique that flicked on special genetic switches called Yamanaka factors to skin cells harvested from middle-aged people in a petri dish. After two weeks, he switched them off and put the skin cells into a culture to promote their growth. Later, Gill measured the age of the skin cells and found that, biologically, they were between 25 and 30 years younger than they had been at the start of the experiment.
Gill and Reik’s experimentation is not being done in isolation. In the past five years, the science of resetting cells has taken off. The promise isn’t merely time travel (albeit on a very, very small scale), but a medical tool that could heal an aging body at the molecular level, regardless of the disease.
“You’re not trying to understand and then treat a specific disease, you’re trying to almost reverse disease in a disease-agnostic fashion,” Reik tells Inverse during an interview from his office in Cambridge, where he is also senior vice president and director of the Cambridge Institute of Altos Labs, a biotech company with $3 billion in financial backing (Jeff Bezos is rumored to be among its investors).
“That’s a very big and very ambitious concept,” he muses. “But if that’s true, that’s super exciting, not only as a scientific concept, but as a concept for the clinic further down the line.”
A Hard Reset
Embryonic stem cells have special properties that enable them to develop into many other kinds of cell.
As we get older, we become increasingly fragile, more prone to the diseases that ultimately end our lives. We’re more susceptible to cancer, heart disease, and lung failure, to name a few of the most deadly risks associated with the inexorable march of time. The treatments for these ailments are often punishing, ineffective, or both.
But in the future, Reik and other scientists believe there may be a way to address these conditions and the underlying causes with one universal solution: pushing the reset button on our cells.
A series of research papers released over the past year reinforce the potential of cellular reprogramming, particularly in the battle against aging and age-related disease. To understand why all of this research is gathering steam now, we need to take a trip back to 2007, when a Japanese scientist at Kyoto University made a breakthrough by unlocking the secret to turn the biological clock back within individual cells.
“You’re trying to almost reverse disease in a disease-agnostic fashion.”
In 2007, Shinya Yamanaka and his team at Kyoto University published a paper reporting the creation of human induced pluripotent stem (iPS) cells from old cells. Pluripotency is the name given to the ability of a stem cell to not only divide and multiply but also be able to change into any cell type in the body. It’s like a Tetris block that can morph into any shape it needs to be.
Yamanaka discovered four genes that, when expressed together, reset a cell from its mature state back to a point where it had the same properties as an embryonic stem cell (an iPS stem cell). So for example, if you have a skin cell taken from an adult human, Yamanaka’s genetic switches could revert that skin cell to tabula rasa, then coaxed to perform a different function. These four genes were dubbed Yamanaka factors, and together, they opened a raft of new possibilities in medical science.
“That was an experimental feat that people really, really admired and thought was an amazing piece of science,” Reik recalls.
Professor Ian Wilmut of the Roslin Institute pictured with “Dolly,” the world’s first cloned sheep.
The Japanese scientist drew inspiration from two breakthroughs decades apart. In 1962, Sir John Gurdon, sometimes described as the godfather of cloning, created a new frog by transferring the nucleus of a tadpole’s intestine cell into the egg of a toad. The success of his project proved that mature cells like the intestine cell still contain the genetic information needed to achieve pluripotency. Otherwise, the egg would never have developed into an organism. This concept was reinforced further by an even more high-profile achievement — the cloning of Dolly the sheep in 1996. He believed there was a set of instructions in the cell, an expression of certain genes, that was able to instruct the cell to return to its pluripotent state.
Yamanaka aimed to solve two issues: create a steady supply of stem cells that won’t fall foul of immune rejection, and avoid the ethical conundrums associated with extracting stem cells from embryos.
Yamanaka’s breakthrough caught the eye of aging researchers. According to Reik, aging expert Steve Horvath kicked things off with a key observation in 2013: He suggested the age of an iPS cell was effectively zero, meaning that aside from erasing a cell’s function, Yamanaka factors also reset its biological age to zero. The hypothesis formed: If scientists could better control the effects of the Yamanaka factors and minimize the risk of side-effects, they may be able to erase some of the effect of aging on the body.
“Would cells know how to become younger and healthier?”
In 2016, scientist Juan Carlos Izpisua Belmonte at the Salk Institute in California made the first major breakthrough in proving this hypothesis: He expressed the Yamanaka factors in mice with progeria, a genetic condition that causes the body to age at an alarmingly rapid rate. The treated animals lived 30 percent longer than a control group, and — crucially — didn’t develop any cancers, one of the biggest risks of using Yamanaka factors.
The iPS cells produced by the Yamanaka factors have all the exceptional properties of embryonic stem cells — able to grow, divide, and become any cell, whether it be a skin, blood, or brain cell. But if they are allowed to develop in the body unchecked, these pluripotent cells cause embryo-like tumors called teratomas. In fact, one of the four Yamanaka factors is a known oncogene, which means it can cause cancer.
Aging researchers like Belmonte discovered that the trick was to limit the capabilities of the Yamanaka factors so the cells don’t fully reach iPS form. This can be done by either expressing the genes for a certain amount of time, expressing only some of the genes and not others, or changing their expression level. In Belmonte’s case, his team switched the genes on for two days a week over several weeks. This has the effect of reversing damage over time, without fully resetting cells.
The Big Question
Pluripotent stem cells may be a tool for scientists to repair damaged tissue.
In the last three years, the science into Yamanaka factors has exploded. In 2020, a team led by David Sinclair used three of the four Yamanaka factors to restore lost sight in mice. Sinclair is a well-known figure in the longevity field who is outspoken in his enthusiasm for extending life beyond the norm. In this study, Sinclair and his team examined the epigenome, the chemical compounds that tell genes what to do and when and where to do it, for signs of aging. In this context, it’s easier to imagine the epigenome as an old-fashioned vinyl record carrying vital instructions. Over time, the record becomes scratched. If you could remove those scratches and restore the record, Sinclair and others believed, you could restore function to the genome and rejuvenate cells.
“The big question was, is there a reset button?” he told Science at the time. “Would cells know how to become younger and healthier?”
The study targeted retinal cells in mice with a harmless virus containing three Yamanaka factors in an attempt to fix a severed optic nerve. The gambit was at least partially successful in restoring function to the retinal cells.
Around the same time, a study co-published by scientists at biotech company Genentech and the Salk Institute showed that expressing the Yamanaka factors in mice in cycles over an extended period of time had no apparent negative health effects on the animals. The study, which was co-led by Heinrich Jasper, who works in immunology discovery at Genentech, also found that partially reprogrammed cells reduced age-related changes in typical, healthy mice, not just those with disease or injury.
“We did this in mice, which doesn’t tell us anything about safety in humans, by the way, but at least we’re able to express these factors systemically in the whole animal for two days a week over the course of about 10 months and the animals are fine and they display some evidence of rejuvenation or delayed aging,” Jasper tells Inverse.
“That’s really what the engineering challenge is right now, based on all the findings that have been made,” he adds. “Can we do something like this in a safe and robust fashion and restore function of cells through a measured expression of these four factors?”
If scientists can overcome that challenge, Jasper believes the technology should be used to treat age-related diseases, not to chase full-body regeneration, Doctor Who style. Jasper uses the example of idiopathic pulmonary fibrosis (IPF), a “classic age-related disease” where the lungs lose their regenerative powers and develop fibrosis.
“The fundamental promise of the four factors is that we should be able to restore the function of, for example, lung stem cells by using this approach and basically reverting them back to a healthier state,” Jasper says. “We haven’t achieved that yet and it’s going to take some time to really prove that, but if we find a way to approach this and control the expression and maybe target some of the downstream nodes, then we might have a way to develop new types of therapies for these types of disease, and that’s really the promise.”
“It’s almost easier to fix something that’s broken than it is to make something that’s good, better.”
In January of this year, the San Diego-based biotech company Rejuvenate Bio released results from another study on reprogramming effects on aging. The company injected elderly mice with a virus that activated three of the Yamanaka factors and found that the animals lived an extra 18 weeks on average, compared to nine weeks for the control group.
Noah Davidsohn, chief science officer and co-founder at Rejuvenate Bio, tells Inverse the paper was significant because it was the first to properly realize some of the potential of the Yamanaka factors. He explains that while previous research has addressed mice with diseases or damage, like progeria or severed optic nerves, this work attempted to make otherwise healthy mice live longer.
“We put it in wild type mice that are really old and are basically the same as really old humans and show that we could increase their life and health span,” he says. “So I think that sparked an ‘Oh wow, it actually does what everyone is promising it’s been doing but hasn’t been done yet.’”
“It’s almost easier to fix something that’s broken than it is to make something that’s good, better,” Davidsohn says.
These types of studies underline the potential of cell reprogramming in the fight against age-related disease, but there is still a lot of work to be done. First, the field needs to understand exactly what is happening on a molecular level when the Yamanaka factors are expressed. This can lead to better control over their expression and will speed up their potential use in humans. Reik at Altos Labs wants to know what kind of cells this kind of treatment will work for.
“Skin is nice because there are some clear changes that happen during aging in the skin that potentially could be addressed in treatment strategies. But could we do this with blood cells, can we do this with heart cells, kidney, whatever — in whichever cell types we experience age-related pathology, which is pretty much all cell types in the body? That’s an interesting question to ask,” he says.
Organoids grown from pluripotent stem cells represent a related avenue of cellular medicine.
“If you think about aging as a biological process that leads to changes in cells, and these changes actually contribute to the incidents and progression of a wide range of age-related, chronic, degenerative diseases,” Jasper says, “then you might really learn something if you’re trying to address these age-related changes and try to modulate them so you have an impact on the progression of a disease, or even on the instances of the disease.”
The promise and potential of the reprogramming field, particularly in relation to aging, has led to increased investment in the area. Jasper estimates there are around 15 to 20 labs working on using the Yamanaka factors together with aging research, and more are emerging every month. “There’s a lot of excitement about potentially what can be done there,” he says.
The Yamanaka factors may never reverse aging in humans, but they could still play an important role in the fight against the multitude of vicious diseases that come with getting older. The number of people aged 80 years or older is expected to triple by 2050, up to 426 million, according to World Health organization figures — and age-related disease will inevitably become more prevalent. As research continues at a steady pace, cellular reprogramming could hold the key to managing that tidal wave of disease looming on the horizon — even if it won’t be applied to making otherwise healthy humans cheat the march of biological time.