The body's internal clock could help explain an incurable brain condition
Circadian rhythm may be a critical mechanism for understanding Alzheimer’s disease.
A good night’s sleep has always been linked to better mood and better health. Now, scientists have even more evidence of just how much sleep — and more specifically our circadian rhythm, which regulates our sleep cycle — is linked to certain diseases, such as Alzheimer’s disease. A team of researchers from the United States has found further evidence that the cells which help keep the brain healthy and prevent Alzheimer’s disease also follow a circadian rhythm.
Our circadian rhythm is a natural, internal process that follows a 24-hour cycle. It controls everything from sleep, digestion, appetite, and even immunity. Things like outside light, when we eat our meals, and physical activity all work to keep our circadian rhythm in sync. But even small things like staying up a bit later than normal, or even eating at a different time than we’re used to can knock this internal “clock” out of whack.
It’s important for our circadian rhythm to work properly, as disruption to this cycle is linked to a number of health problems, including mental health conditions, cancer, and Alzheimer’s.
Research shows that for patients with Alzheimer’s disease, circadian rhythm disruptions are usually seen as changes in a patient’s sleep habits that happen long before the disorder fully manifests. This is something that gets worse in the later stages of the disease. However, it’s not yet fully understood whether poor sleep causes Alzheimer’s, or if it happens as a result of the disease.
Circadian rhythm and the brain
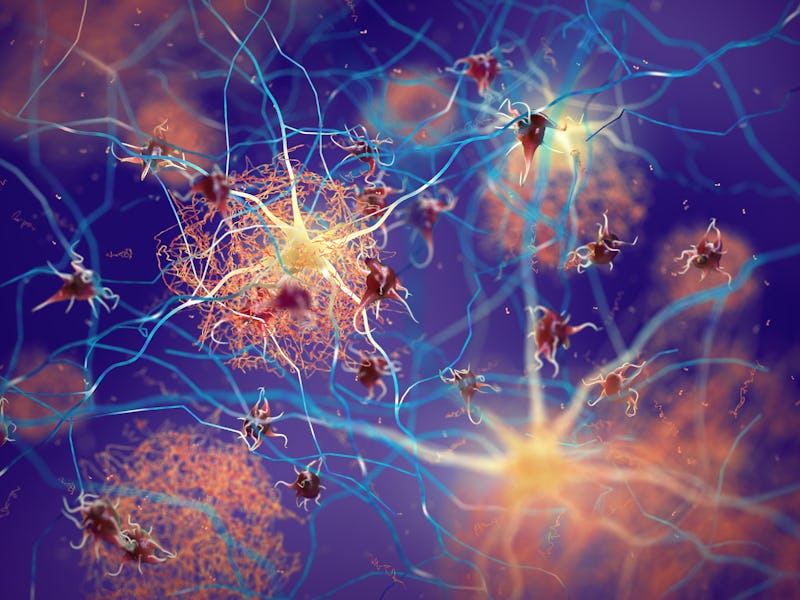
One thing researchers consistently find in the brains of people with Alzheimer’s disease is an accumulation of a protein called beta-amyloid. These proteins tend to clump together in the brain and form “plaques”. These plaques disrupt the function of the brain’s cells, which may, in turn, lead to cognitive issues, such as memory loss. In normal brains, the protein is cleaned up before it has the chance to cause issues.
This latest study has now shown that the cells responsible for clearing up beta-amyloid plaques – and keeping the brain healthy — also follow a 24-hour circadian rhythm. This could mean that if the circadian rhythm is disrupted it could make it more difficult for these cells to remove the harmful plaques that are linked to Alzheimer’s.
The circadian rhythm is a natural, 24-hour cycle that controls many of the body’s processes.
To conduct their research, the team looked specifically at macrophages. These are immune cells that exist throughout the body, including in the brain. Macrophages essentially eat up anything (such as bacteria, or even proteins that haven’t formed correctly) that might be considered a threat to the body.
To understand whether these immune cells follow a circadian rhythm, the researchers used macrophages from mice and grew them in the lab. When they fed the cells with beta-amyloid, they found that the ability of the macrophages to eliminate beta-amyloid changed throughout a 24-hour period.
They also found that specific proteins on the surface of the macrophages — called proteoglycans — have a similar circadian rhythm throughout the day. In fact, they found that when the number of proteoglycans was at their lowest levels, beta-amyloid clearance was at its highest. So when the macrophages have a lot of these proteins, they don’t clear beta-amyloid as well. They also found that when the cells lost their natural circadian rhythm, they didn’t clear beta-amyloid as normal.
Although this study used mouse macrophages that weren’t brain-specific, other studies have shown that microglia — the brain’s immune cells (which are also one type of brain macrophages) — also have a circadian clock. This circadian clock regulates everything from the function and morphology of microglia to its immune response.
It’s possible that microglial circadian rhythm may also even be involved in the control of neuronal connectivity — which eventually might contribute to the worsening of Alzheimer’s-related symptoms, or even sleep issues that older people might exhibit.
What this means for humans
But in studies that have looked at full organisms (such as mice) instead of only cells, the results about the relationship between Alzheimer’s and circadian rhythm are more conflicting — they often fail to portray all the issues found in humans with Alzheimer’s disease, as they only study specific systems or proteins that might be affected by Alzheimer’s disease. This means they aren’t a fully accurate representation of how Alzheimer’s occurs in humans.
In studies that looked at people with Alzheimer’s, researchers have found that circadian rhythm dysfunction has worsened as the disease progressed. Other research also showed that this circadian rhythm disruption was linked with sleep problems and Alzheimer’s disease, alongside the brain being less able to clear brain “garbage” (including beta-amyloid) — which may further contribute to memory problems. But it’s difficult to say whether circadian rhythm disruption (and the problems it causes) happened as a result of Alzheimer’s disease, or if they were part of the cause.
Should the findings of this study be replicated in humans, this could bring us one step closer to understanding one of the ways in which our circadian rhythm is linked to Alzheimer’s disease. Nevertheless, it’s widely agreed that sleep is important for many aspects of our health. So protecting your circadian rhythm is not just good for your brain — but for your overall health.
This article was originally published on The Conversation by Eleftheria Kodosaki at Cardiff University. Read the original article here.