Why the future of treatment-resistant depression is bound to the immune system
An “important molecule of interest” is a bridge between two competing ideas.
The FDA approval and emergence of selective serotonin uptake inhibitors (SSRIs) in the late 1980s transformed psychiatry. Finally, there was an effective and inexpensive medication for depression, a leading cause of disability worldwide. Today SSRIs are some of the most widely prescribed drugs.
However, as scientists report in a recent paper published in the Journal of Neuroscience, interest in SSRIs within the research community has diminished. This is because these drugs, known by brand names like Prozac and Zoloft, exhibit “variable clinical efficacy” — they don’t work for everyone. A growing number of people experience treatment-resistant depression, or TRD.
This has spurred a revolution in mental health research, prompting scientists to explore taboo substances like ketamine and MDMA as therapeutics for depression.
But in the Journal of Neuroscience paper, researchers at Imperial College London and the University of South Carolina argue a path forward doesn’t have to mean counting out SSRIs, but tweaking their application. Their argument stems from one of the most fundamental reactions experienced by the body: inflammation.
Why? The study team found histamines, molecules involved in the immune system and present in the brain, are an important link between depression and inflammation because of their effect on serotonin. In the long view — and more research is needed to know for sure — this work suggests antidepressants like SSRIs may work more efficiently for some if paired with novel drugs that reduce histamine in the brain.
Histamine, explains co-author, post-doctoral fellow, and student leader of the project Melinda Hersey, plays a role in both mediating the immune response (like the release of cytokines) and ability to modulate monoamine neurotransmitters (like serotonin) believed to be altered in depressed individuals.
It is “an important molecule of interest,” she tells Inverse. And it’s a bridge between two competing ideas for the cause and treatment of depression.
The competing depression hypotheses
To understand why the histamine connection is novel, you have to know the two classical hypotheses of depression: the monoamine hypothesis and the cytokine hypothesis. (These are eloquently explained in an accompanying review written by Hersey and colleagues in the European Journal of Neuroscience.)
1. The monoamine hypothesis of depression
This is the explanation of depression you likely know. It’s the idea that monoamines — the neurotransmitters dopamine, serotonin, and norepinephrine — are dysregulated during depression. This theory arose when researchers examined the blood, urine, and cerebral spinal fluid of depressed patients, and found monoamines and their metabolites were decreased.
Prozac capsules: Fluoxetine, brand name Prozac, is used to treat depression, OCD, some eating disorders, and panic attacks.
This hypothesis is also supported by the fact that SSRIs still work for many. These drugs are designed to allow serotonin to circulate for longer in the brain and improve mood. Still, there’s a growing appreciation for the fact that, for some people, SSRIs aren’t helpful enough and/or come with adverse side effects.
“There is an emerging appreciation that the heterogeneity of response to antidepressant drugs that target the monoamine system reflects the overall heterogeneity of depressive illness,” the team writes.
2. The cytokine hypothesis of depression
Studies also point to pro-inflammatory cytokines as a factor in the development and progression of depression. Historically, scientists thought the brain wasn’t influenced by cytokines, because of the blood-brain barrier. (Inflammatory cytokines are signaling molecules that promote inflammation.)
Now, researchers know it's not immune: inflammatory cytokines can influence brain chemistry associated with psychiatric disorders.
Meanwhile, a number of illnesses characterized by chronic inflammation, like rheumatoid arthritis, are now understood to be accompanied by depression. Depression itself is associated with a chronic, low-grade inflammatory response.
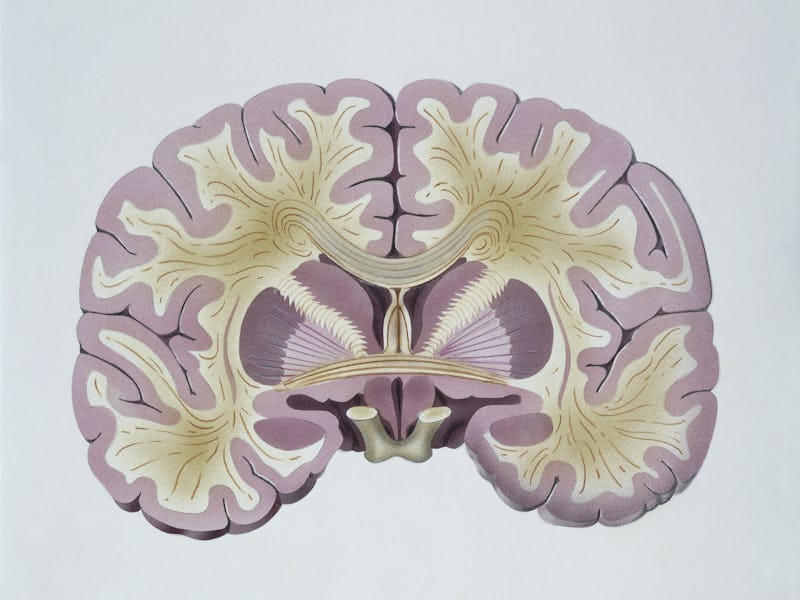
A model of the human brain.
“It is fairly well established that depression is associated with inflammation, as most patients with depression have also been shown to have elevated inflammation markers,” Hersey says.
An acute immune reaction known to produce a “sickness behavior” in humans and in rodents is also accompanied by “symptoms that mirror depression or depressive-like phenotypes,” Hersey adds.
Depressed patients with severe inflammation are among those most likely to not respond to SSRIs.
But two factors prevent an “a-ha” moment: this inflammation hypothesis alone cannot “sufficiently explain the pathophysiology depression.” SSRIs also have anti-inflammatory properties.
What’s possible, the study team contends, is that these hypotheses actually overlap.
Enter histamines, stage left.
The experiment — The team had a hunch it was the relationship between serotonin and histamine that made it difficult for those with TRD to benefit from SSRIs.
So they took mice and implanted biocompatible serotonin-measuring microelectrodes into the hippocampus of their brains. This allowed the scientists to measure brain serotonin levels without harming the brains.
Then, half the mice were injected with an inflammation-causing toxin, with the rest left as controls. Within minutes, brain serotonin levels dropped in the injected mice. Because this toxin is known to be unable to cross the blood-brain barrier, it was clear that it was not causing this directly.
What could cause the drop, however, is histamine: Analysis revealed the inflammatory response triggered histamine release, which in turn attached itself to neurons and inhibited the release of serotonin.
When they gave the mice SSRIs they still couldn’t boost serotonin levels. It was only after the administration of histamine-reducing drugs that serotonin levels returned to normal. (These drugs are not the same as antihistamines.)
What comes next — While this work is what’s considered preclinical data — it involved mice, not humans — the team hopes it can eventually provide a new avenue for treatment, taking form as a therapeutic targeting both histamine and serotonin. They want to “alleviate depressive symptoms even among individuals with treatment-resistant depression,” Hersey says.
The next chapter will focus on three main areas of focus, she says:
- Exploring how chronic inflammation may affect the serotonin-histamine relationship
- Performing an in-depth characterization of histamine in the brain
- Observing histamine and serotonin dynamics within human stem cells
But questions remain, including a chicken-and-egg situation: Does inflammation lead to depression, or does depression lead to inflammation?
It’s likely both. Depression, Hersey explains, “is a very heterogeneous disease” so it’s possible “disease pathology may proceed in a variety of ways on a case-by-case basis.”