The virus that causes cold sores could trigger a devastating brain condition
Oral herpes is one of the most common viruses in the world.
Herpes simplex virus type 1 (HSV-1) is the kind of herpes that causes cold sores on your mouth. But while uncomfortable on the outside of your face, scientists are increasingly concerned about what the virus does on the inside of your skull. There, according to new research, it may have links to a devastating brain condition.
In 3D models of human brains, scientists found that HSV-1 can trigger buildup that resembles amyloid plaques. These are sticky clumps of proteins that tend to accumulate between the neurons of Alzheimer's disease patients. In turn, these clumps pave the way for a slow decline in memory and cognitive skills.
This finding was published Wednesday in the journal Science Advances.
The study suggests a powerful and complex connection between Alzheimer's and one of the most common viruses on Earth (and oddly, in space). The World Health Organization estimates that 67 percent of the global population under 50 has HSV-1.
It's also incurable: Once a body is infected, the virus lingers and can flare up every so often. This causes cold sores.
The fact that the virus lingers in the system could partially explain why there's an increasingly understood connection between HSV-1 and Alzheimer's, explains David Kaplan. Kaplan is the study's senior author and director of Tufts University's Tissue Engineering and Research Center.
A working hypothesis is that the virus triggers an immune response in the brain, causing it to create those plaques in order to "trap" the virus, Kaplan says. At first, that response actually works. But later on, this defense mechanism goes awry.
"While the initial formation of amyloid-beta is beneficial for clearing infection, over time, these proteins aggregate to form plaques which themselves eventually become toxic to cells of the brain," Kaplan explains.
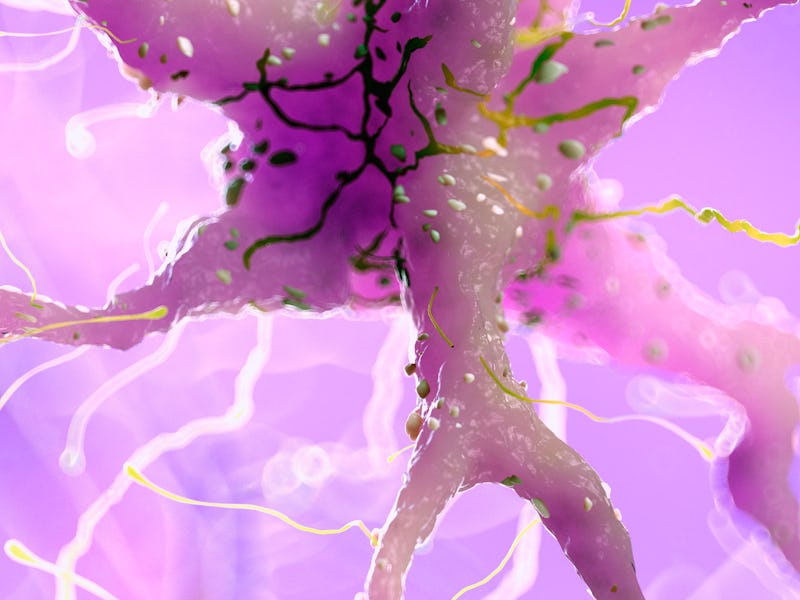
After 3 days of HSV-1 infection, 3D brain models developed Alzheimer's-like plaques (seen in green and pink).
Herpes and the brain – Thirty years ago, scientists in England noticed that genetic signs of the herpes virus lingered in the brains of Alzheimer's patients at much higher rates than in healthy patients. Since then, several studies have strengthened a connection between HSV-1 and Alzheimer's, especially in patients who have severe herpes cases.
However, in January 2020 a large study published in Neuron called this connection into question. After screening 711 brains of Alzheimer's patients and healthy controls, scientists found no evidence that the patients had increased levels of herpes RNA. However, they couldn't rule the connection between herpes and Alzheimer's out entirely. Looking at the brain of someone after they've died can't always reveal what was happening during the early stages of the disease.
This new study was intended to help clarify how the herpes virus might lead someone down the path to Alzheimer's, even if there was no family history of the disease.
Kaplan and his team developed models of human brain tissue using stem cells. Models aren't perfect analogs to the human brain, but they get close: This 3D model was still replete with synapses, connections between brain cells that allow them to communicate.
That allowed them to approximate a working human brain. Kaplan still notes "a real brain is still much more complex."
Importantly, these brain models are intended to look like healthy brains. Investigating healthy models helps clarify how herpes might be linked to Alzheimer's in a person that has no genetic risk from their family tree. In fact, most Alzheimer's cases don't actually run in families. These are called "sporadic Alzheimer's disease."
After "infecting" the models with low levels of the herpes virus (high levels actually killed the cells), the team noticed amyloid plaques developed within three days. In tandem, the electrical activity within the model significantly dropped off compared to controls. That suggests that the brain began to operate as if it had been hampered by Alzheimer's.
As far as Kaplan knows, that was the first example of a sporadic Alzheimer's case in a once-healthy model brain. Because these cells weren't taken from someone who already had the disease or from someone with a family history, the experiment revealed one way the brain can develop Alzheimer's in the presence of the herpes virus.
This demonstration could help develop treatments for the disease in the future, Kaplan says. When the brain developed Alzheimer's, they noticed that certain genes were turned on. Those genes, he says, are likely the same ones involved in the development of early-onset Alzheimers (when symptoms show up before age 65).
"It's plausible that these up-regulated genes could be potential targets for future drug interventions to halt the progression of the disease," Kaplan adds.
Of course, simply having one of the most common viruses on earth isn't a guarantee of developing Alzheimer's. But if the connection continues to be strengthened, it could provide one answer for why some people experience a change in the brain later in life.
Abstract: Alzheimer’s disease (AD) is a neurodegenerative disorder that causes cognitive decline, memory loss, and inability to perform everyday functions. Hallmark features of AD—including generation of amyloid plaques, neurofibrillary tangles, gliosis, and inflammation in the brain—are well defined; however, the cause of the disease remains elusive. Growing evidence implicates pathogens in AD development, with herpes simplex virus type I (HSV-1) gaining increasing attention as a potential causative agent. Here, we describe a multidisciplinary approach to produce physiologically relevant human tissues to study AD using human-induced neural stem cells (hiNSCs) and HSV-1 infection in a 3D bioengineered brain model. We report a herpes-induced tissue model of AD that mimics human disease with multicellular amyloid plaque–like formations, gliosis, neuroinflammation, and decreased functionality, completely in the absence of any exogenous mediators of AD. This model will allow for future studies to identify potential downstream drug targets for treating this devastating disease.