Can vaccines help protect the gut? Fungus study hints at future treatments
Fungi are important members of the microbiome — but they can also hurt human health.
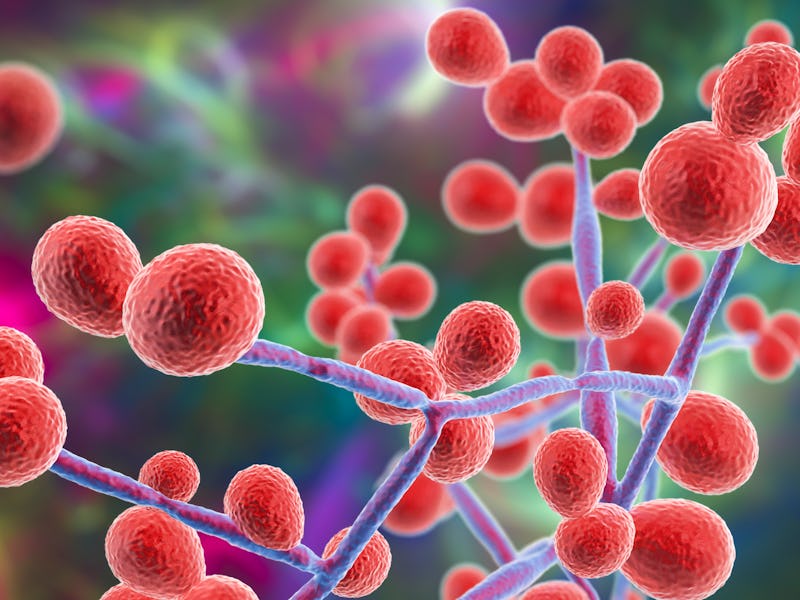
If you hitched a ride onto Ms. Frizzle’s Magic School Bus, a trip inside the human body would reveal your digestive system hard at work as microorganisms of all shapes and sizes do their thing. One important and often overlooked population within the gut microbial community is fungi. Fungi are a double-edged sword — they are critical to health but they can also turn into an intestinal instigator of infections.
To stop fungi from going to the dark side, a team of researchers led by Kyla S. Ost from the University of Utah School of Medicine, are developing a fungal vaccine to treat inflammatory bowel disease.
INVERSE is counting down the ten most-surprising discoveries about your wondrous gut in 2021. This is #5. Read the original story here.
What’s new — The team’s vaccine has so far been developed and tested in a mouse model mimicking IBD. Their findings, published earlier this year in the journal Nature, show that the vaccine could treat IBD by blocking a fungal species called Candida albicans converting from harmless to harmful.
Ost and her colleagues discovered that the mice’s immune response to Candida albicans could help distinguish between benign and pathogenic fungi.
“What we found was a number of these sticky molecules called adhesions, which function to facilitate adherence and sometimes invasion of host tissue,” Ost explains.
Expressing these adhesions harmed the mice’s gut health, but certain antibodies could target these molecules, and in turn, the pathogenic version of Candida albicans.
The vaccine also increased the immune response to the pathogenic fungi and lessened fungi-related damage in the intestines.
Candida albicans also causes yeast infections, like thrush.
How they did it — “Fungi are wonderfully complex and dynamic organisms, often capable of dramatically changing their morphology and their biology and in the face of different stresses and conditions within the host,” Ost tells Inverse.
“I was really interested in how the immune system detects and sort of changes fungi’s pathogenic potential. So, how does the immune system stop these fungi from becoming pathogenic within the gut?”
Fungal species are normal inhabitants of the intestinal microbiota, but they also cause infections and exacerbate inflammatory diseases such as IBD.
To start, the researchers surveyed a number of different fungal species and their ability to provoke an intestinal adaptive immune response such as an antibody response. They opted to take a closer look at Candida albicans because it is one of the fungal species that elicits a large immune response.
Candida albicans can exist in two forms. It is found in most healthy people, Ost says, but one of its forms — a “hyphal” form that causes distorted cell shapes — is strongly associated with disease.
“[Candida albicans] is documented to be one of the most pathogenic fungi within the gut, meaning it can cause disseminated infections if allowed to escape this site,” she adds.
Why it matters — The vaccine blocked the Candida albicans from causing disease — which could be potentially protective against IBD, Ost says.
The vaccine has not been tested in people with IBD. But Candida albicans is also the fungus that causes vaginal yeast infections, so Ost says there are clinical trials underway to use a similar protocol for the treatment of recurrent vaginal yeast infections. That means researchers know the vaccine is safe in humans — an important step to testing it for IBD.
“This vaccine has been through a number of human clinical trials for safety and could potentially be repurposed for people with IBD to block these fungi from exacerbating their disease,” Ost says.
This article was originally published on