A link between fungi and gut health may mean a treatment for inflammation
Scientists find “sophisticated communication” between fungi and our immune system.
Gut bacteria tend to seize the spotlight in conversations about gut health.
It’s known changes in gut bacteria influence wellness, and probiotics are meant to help the “good” bacteria. But other little organisms exist within the gastrointestinal tract, including one both influential and too often forgotten: fungi.
Fungi is with us wherever we go, living in harmony with the systems of our body — usually.
A study published Wednesday in Nature explores the difference between fungi that harm and fungi that benefit gut health, finding the body is prepared to fight off potential foes. Our body’s immune response can actually target the more dangerous form of common gut fungi, the study suggests. This, in turn, strengthens the more beneficial form.
In an experiment involving mice, the study team also used a vaccine to demonstrate the possibility of future treatment. If later studies prove successful, it’s possible a similar vaccine could treat forms of irritable bowel disease, like Crohn’s disease, by capitalizing on the precision of this immune system response.
What you need to know first — Fungi make up only about one percent of our gut microbiome. They’re far outnumbered by bacteria and other microbes.
But according to Kyla Ost, fungi also “play a really outsized role in shaping immune responses impacting host health.” Ost is the lead author of the study and a postdoctoral researcher at the University of Utah.
Fungi have been suspected of playing a role in the development of inflammatory bowel disease (IBD), but the connection between the fungi and disease so far hasn’t been clear. In “healthy” guts, some fungi can coexist peacefully with the rest of our digestive system. But, in some guts, the same little organisms can also exacerbate inflammatory diseases.
The researchers already knew the body’s antibody responses kept some microbes in the gut in check, so they were curious: Did the same apply to fungi?
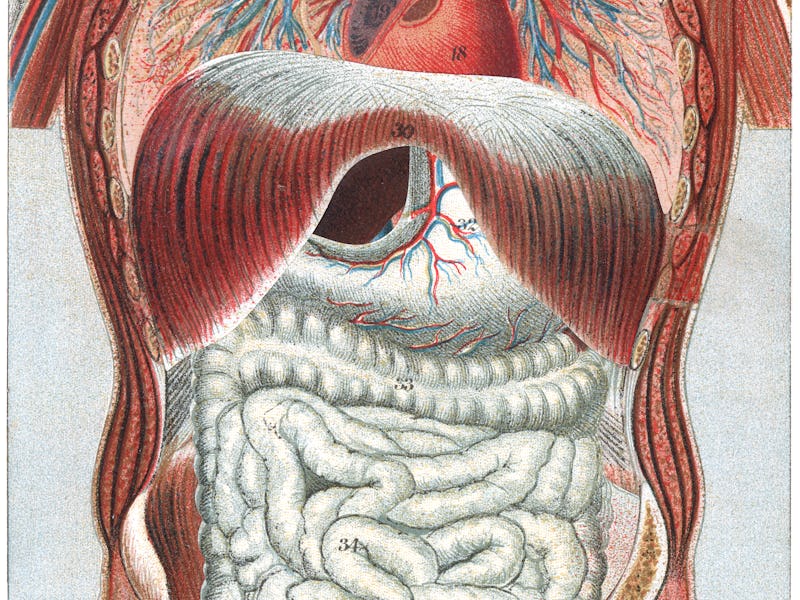
Candida albicans, the most common fungi found in the gut.
The study process — In a mouse study, the team confirmed human gut antibodies can affect certain kinds of fungi found in the microbiome. One of the most common fungi in the gut, Candida albicans, elicited an especially large immune response.
Candida albicans can exist in two forms. One is a benign yeast form made up of one cell. The other is “hyphal” — this is when the cells become oblong, elongated shapes called hyphae.
The elongated form may be more pathogenic in guts with IBD — that is, more likely to lead to disease — because certain molecules which form on them make them better able to stick to host cells.
“... there is this really sophisticated communication between these commensal fungi within the gut and our immune system.”
When the scientists looked more closely at the immune response, they found certain antibodies in the intestine targeted the pathogenic, hyphal form of the Candida. This process ultimately benefited the benign yeast form in the gut. Ost referred to this kind of control over a fungi population by the immune system as “immune sculpting.”
Using a vaccination in mice with an IBD-like disease, the researchers were able to increase the immune response to the pathogenic forms of the Candida albicans and the mice showed less fungi-related damage to their intestines.
What’s new — The investigation revealed immune systems are able to distinguish the benign and harmful forms of the fungi, Candida albicans.
They also found a vaccine given to mice could actually increase the immune response to fungi in its pathogenic form.
“We've demonstrated that you can use vaccination to, in a very selective way, block the pathogenic effects without disrupting the microbiota as a whole — which we know is very beneficial for many aspects of our health,” Ost says.
Why it matters — First, there’s the scientific significance. Fungi — not just bacteria or other microbes in the gut — interact in a complex way with our immune system.
“I was totally fascinated by the fact that there is this really sophisticated communication between these commensal fungi within the gut and our immune system,” Ost says. “Most microbiota researchers think of these microbes within our gut as static organisms that are not adapting themselves.”
Using knowledge of this interaction, the team was able to apply a vaccine that reduced intestinal damage in mice with an IBD-like condition, caused by the Candida fungi type that can lead to disease. The vaccine boosted an antibody response that targeted the “sticky” molecules on the oblong fungi forms and protected the mice from symptoms.
What’s next — Ost wants to find out exactly how the vaccine was working. The vaccine didn’t seem to just prompt the immune system to eliminate the “bad” forms of the Candida fungi — something more complex appears to be going on. But what exactly, is unclear.
The study also suggests it may be time to reevaluate what gut health really means.
“I hope that this study and the attention that it's getting will remind people that fungi are within our gut, and they're also important organisms to think about,” Ost says.
Abstract: Pathogenic fungi reside in the intestinal microbiota but rarely cause disease. Little is known about the interactions between fungi and the immune system that promote commensalism. Here we investigate the role of adaptive immunity in promoting mutual interactions between fungi and host. We find that potentially pathogenic Candida species induce and are targeted by intestinal immunoglobulin A (IgA) responses. Focused studies on Candida albicans reveal that the pathogenic hyphal morphotype, which is specialized for adhesion and invasion, is preferentially targeted and suppressed by intestinal IgA responses. IgA from mice and humans directly targets hyphal-enriched cell-surface adhesins. Although typically required for pathogenesis, C. albicans hyphae are less fit for gut colonization1,2 and we show that immune selection against hyphae improves the competitive fitness of C. albicans. C. albicans exacerbates intestinal colitis3 and we demonstrate that hyphae and an IgA-targeted adhesin exacerbate intestinal damage. Finally, using a clinically relevant vaccine to induce an adhesin-specific immune response protects mice from C. albicans-associated damage during colitis. Together, our findings show that adaptive immunity suppresses harmful fungal effectors, with benefits to both C. albicans and its host. Thus, IgA uniquely uncouples colonization from pathogenesis in commensal fungi to promote homeostasis.
This article was originally published on