The Covid-19 pandemic has reshaped the lives of smokers acutely aware of its ability to wreak havoc on the lungs. In March, hopeful quitters told Inverse they were eager to stop smoking as cases surged.
Those smokers acted prudently. New research reveals exactly what they had to gain from quitting: avoiding fundamental changes in lung cells that can make it harder for Covid-19 to take hold.
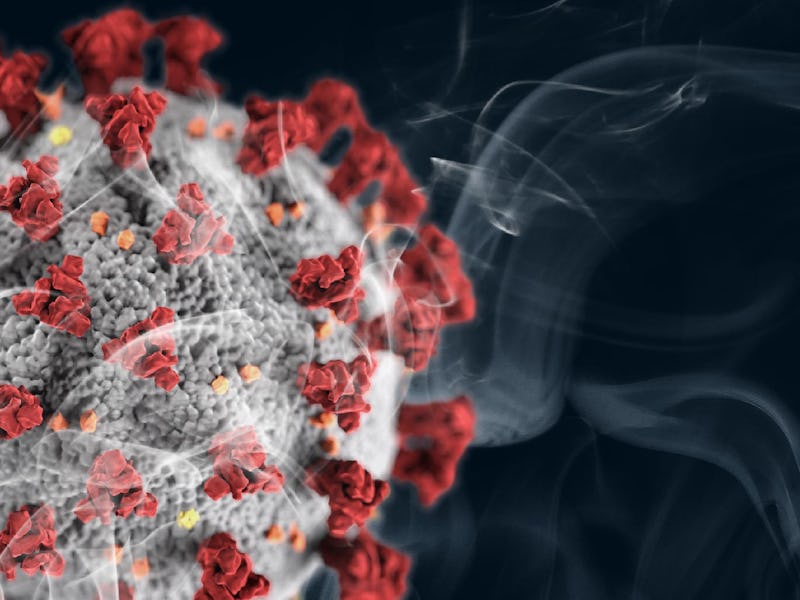
The virus that causes Covid-19 — SARS-CoV-2 — needs two elements to latch onto a cell. These are a spike protein (the spiky exterior that looks like a crown) and an ACE-2 receptor, an enzyme that lingers on the cell's surface. In turn, the spike protein attaches to the ACE-2 receptor.
Cigarette smoking actually increases the amount of ACE2 receptors in the lungs, reveals a study published last week in Developmental Cell.
The study is a survey of human and animal research, and taken together, suggests that smoking increases the number of landing pads for Covid-19 in the body. The overabundance of these cells could partially explain why smokers are more likely to get severe cases of Covid-19, the authors explain.
Jason Sheltzer is a fellow at the Cold Spring Harbor Laboratory and the paper's corresponding author. He tells Inverse that while we still don't know for sure that ACE2 expression is linked to more susceptibility to Covid-19, the overexpression of ACE2 has been theorized as a risk factor.
"It's possible that ACE2 has some beneficial functions as well," says Sheltzer.
Even with the nature of ACE2 over-expression unknown, this paper jibes with additional work suggesting that smoking and Covid-19 don't go well together. ACE2 expression may end up being part of that much larger story.
"These results may partially explain why smokers are particularly susceptible to severe SARS-CoV-2 infections," Sheltzer and his team write.
The case for ACE2 – Some studies suggest that increasing ACE2 expression allows the coronavirus to take hold in the body, and cause more severe disease. For instance, a pre-print study from China (not peer-reviewed) analyzed 700 lung tissue samples from severe Covid-19 patients who had underlying conditions, like hypertension, diabetes, and chronic obstructive lung disease. Those patients had high levels of ACE2 expression in common.
"These results may partially explain why smokers are particularly susceptible to severe SARS-CoV-2 infections."
This analysis pulls data from previous studies on both humans and animals to confirm the links between ACE2 expression and smoking.
The team reanalyzed data from smokers and non-smokers collected in 2009, 2011, and 2017. Across those samples, human smokers expressed between 30 and 55 percent more ACE2 receptors in their lungs than non-smokers did.
The team also reports that the genes responsible for ACE2 expression tend to be over-expressed after a viral infection. In two studies that investigated the coronaviruses that cause SARS and MERS, the team found that ACE2 expression increased post-infection with each virus.
If the virus itself can increase ACE2 expression and smokers already have higher levels of those receptors to start with, the problem can become compounded, the study suggests.
Sheltzer explains that smoking tends to increase a form of respiratory cell called a goblet cell, which secretes mucus and helps clear the lungs (that mucus is also responsible for the smoker's hacking cough).
Those mucus-producing cells, however, also tend to produce additional ACE2 receptors, Sheltzer says.
"The same cells that produce mucus also express ACE2, so ACE2 expression increases as mucus production increases," he explains.
If ACE2 expression, smoking, and coronavirus are actually as tightly tied as this study suggests, then scientists may have found yet another reason why quitting can be somewhat protective. Sheltzer notes that, in data collected from people who quit smoking, they found that ACE2 receptors reduced by as much as 40 percent after one year.
The big picture – This study establishes that smoking is associated with both higher ACE2 levels and worse coronavirus symptoms. What still needs to be established is whether it is exactly the higher ACE2 levels that's actually driving the worse symptoms.
Despite studies in Wales and France looking into nicotine patches as Covid-19 treatment, the overwhelming picture is that smoking and coronavirus don't mix. (These studies still note that smoking enhances the risk of worse Covid-19 symptoms, regardless of the amount of nicotine in a cigarette.)
In May, the World Health Organization released a statement noting that smokers are more at risk of severe Covid-19 cases. Meanwhile, high rates of smoking have been partially blamed for Indonesia's high Covid-19 death rate. Early studies in China suggested that smokers were 14 times more likely to need intensive treatment for Covid-19.
We also know that smoking can depress the immune system (as does vaping) which could lead to greater susceptibility to Covid-19 infections. Panagis Galiatsatos, an associate professor at Johns Hopkins and spokesperson for the National Lung Association, previously told Inverse that vapers are more likely to have "dire consequences" from Covid-19 than non-vapers.
Sheltzer also theorizes that vaping could increase susceptibility to Covid-19, though his study doesn't speak to it directly. "Things that irritate the lungs would probably on balance be harmful," he says.
Coronavirus and ACE2 may provide the extra impetus to quit, but the long-term risks of smoking have been around long before the pandemic crystallized them. Still, the unique, and developing relationship between coronavirus and smoking make quitting a more relevant than ever.
Abstract: The factors mediating fatal SARS-CoV-2 infections are poorly understood. Here, we show that cigarette smoke causes a dose-dependent upregulation of Angiotensin-Converting Enzyme 2 (ACE2), the SARS-CoV-2 receptor, in rodent and human lungs. Using single-cell sequencing data, we demonstrate that ACE2 is expressed in a subset of secretory cells in the respiratory tract. Chronic smoke exposure triggers the expansion of this cell population and a concomitant increase in ACE2 expression. In contrast, quitting smoking decreases the abundance of these secretory cells and reduces ACE2 levels. Finally, we demonstrate that ACE2 expression is responsive to inflammatory signaling and can be upregulated by viral infections or interferon treatment. Taken together, these results may partially explain why smokers are particularly susceptible to severe SARS-CoV-2 infections. Furthermore, our work identifies ACE2 as an interferon-stimulated gene in lung cells, suggesting that SARS-CoV-2 infections could create positive-feedback loops that increase ACE2 levels and facilitate viral dissemination.