Cocaine study reveals how unseen brain changes lead to relapse
A study on addicted mice could serve addicted humans in the future.
Cocaine is so powerfully addictive that quitting it can be incredibly difficult, especially since there are no approved medications to ease the process. To prevent relapse, people turn to exercise or pray for a future vaccine. But according to early-stage research, scientists are trying a new tactic — there might be a way to stop these relapses before they even happen.
A new study examines cocaine's effects deep in the brain, illuminates how it rewires it, and shows us how tiny, unseen changes become the prelude to a drug relapse.
Cocaine's characteristic high comes back to how the drug keeps the brain flooded with dopamine, the brain's major reward system neurotransmitter. When a team of scientists studied cocaine-addicted mice, they revealed another aspect of dopamine that cocaine exacerbates: In the brains of these mice, dopamine caused lasting changes to their genes.
That may not seem like much, but these tiny molecular changes underpin far bigger sets of behaviors, including drug relapse, explains senior author Ian Maze. Maze is a neurobiologist at Mt. Sinai's Icahn School of Medicine.
"It is becoming more and more clear that molecular alterations in the brain occur during attempted abstinence from drugs of abuse," Maze tells Inverse. Those changes tend to act as precursors to relapse, he explains.
Maze explains that a "major focus" in his field is to try to find out what these changes are, and find ways to target and reverse. This, he hopes, is how we can stop relapses from happening in the future.
The signs of a relapse could appear in the brain before it even happens.
The prelude to a relapse – In the first year after deciding to quit, relapse can be a plague.
A 1999 study found that 23.5 percent of cocaine users start using at least once per week, one year after they leave addiction treatment. Other research suggests that relapse can continue to haunt people even after the physical symptoms of the drug subside — simply spending time away from a drug does not mean that relapse won't happen.
This new study suggests that the urge to relapse begins with changes to a structure called a histone. Histones are collections of proteins that act as spools for DNA (it's wound around histones like twine).
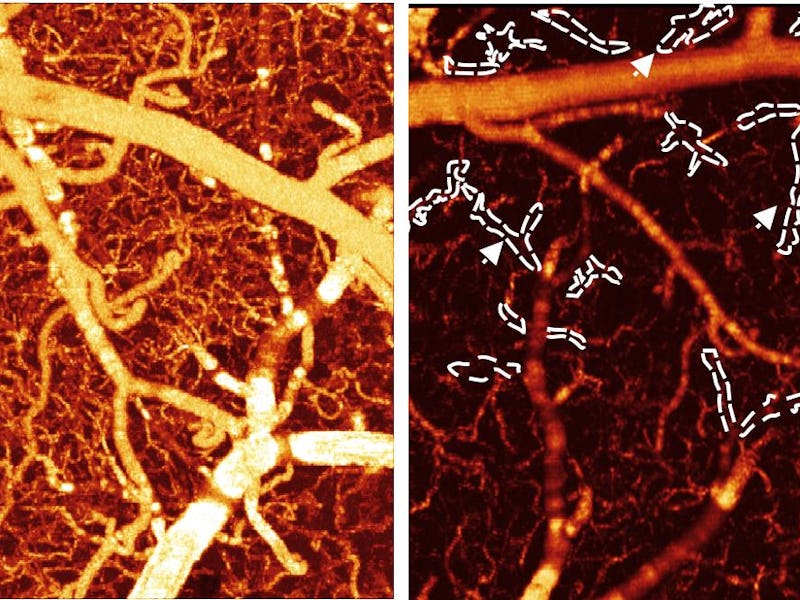
Maze and his team report that dopamine can actually attach to the ends of those histones, which changes the way the genes housed on them are expressed. These changes then alter the firing of neurons in the ventral tegmental area, which is full of dopamine-releasing neurons. This sets a vicious cycle in motion where dopamine both creates changes and is affected by those changes.
Maze's study suggests that this vicious cycle wreaks havoc in the brains of mice with a cocaine problem.
When mice were allowed to have as much cocaine as they wanted for 10 days, the dopamine-related changes to histones dropped off. However, after one month of cocaine withdrawal, the team found that these histone-related changes spiked.
What could reverse the changes was using a lot of cocaine once again (again, the mice had unlimited access to the drug). Food or even limited amounts of the drug didn't reverse the changes. The brain had been prepped to relapse to return to its new, dopamine-rich, normalcy.
What can stop a drug relapse?
In follow-up experiments, the team tried to stop these precursor steps from happening.
To do that, they injected mice with a virus that stopped dopamine from attaching to the histones. Then, mice were prevented from accessing cocaine.
In response, neurons in the ventral tegmental area didn't fire as often and dopamine levels in the brain decreased. But, most importantly, they found that the mice didn't seek out the drug when they were deprived of it.
By stopping dopamine from attaching to histones, the scientists were able to prevent drug relapse by stopping changes in the brain that drive mice to seek out drugs. Taken together, Maze hopes that we might be able to use this research to prevent relapse in humans in the future.
"It is our hope that we will be able to use this information to eventually develop strategies for targeting these processes directly in human drug dependents," Maze says. "Although, as with all basic findings, much more work needs to be done."
This is the first step. If the echoes of relapse can be heard before it actually arrives, scientists and cocaine users alike may have a good chance at fighting it off.
Abstract: Vulnerability to relapse during periods of attempted abstinence from cocaine use is hypothesized to result from the rewiring of brain reward circuitries, particularly ventral tegmental area (VTA) dopamine neurons. How cocaine exposures act on midbrain dopamine neurons to precipitate addiction-relevant changes in gene expression is unclear. We found that histone H3 glutamine 5 dopaminylation (H3Q5dop) plays a critical role in cocaine-induced transcriptional plasticity in the midbrain. Rats undergoing withdrawal from cocaine showed an accumulation of H3Q5dop in the VTA. By reducing H3Q5dop in the VTA during withdrawal, we reversed cocaine-mediated gene expression changes, attenuated dopamine release in the nucleus accumbens, and reduced cocaine-seeking behavior. These findings establish a neurotransmission-independent role for nuclear dopamine in relapse-related transcriptional plasticity in the VTA.