CRISPR cell therapy could turn bad fat into good fat
A proof-of-concept method may revolutionize the way we treat obesity.
Since 1976, worldwide obesity has nearly tripled. This complex, chronic disease continues to be on the rise, especially among children.
Obesity, defined by the Centers for Disease Control and Prevention as having a body mass index (BMI) over 30, occurs when the body stores too much white fat and not enough brown fat. The latter is the so-called "good" kind of fat — it burns energy to help maintain body temperature.
Researchers recently discovered a novel way to fight obesity — tricking white fat into acting more like brown fat, and in turn, burning higher levels of energy. Although the research was conducted on human cells transplanted into mice, the new cell therapy, which hinges on CRISPR technology, could lead to a totally new way of treating obesity, diabetes, and metabolic disorders in people.
"The most exciting part is we now are able to use CRISPR technology to turn the so-called 'bad fat' into 'good fat,'" study co-author Yu-Hua Tseng, obesity and diabetes researcher at Harvard's Joslin Diabetes Center at Harvard University, tells Inverse.
Tseng and her team's research was published Wednesday in the journal Science Translational Medicine.
The difference between white and brown fat
For years, scientists have understood "not all fat tissues are bad," Tseng explains.
In contrast to its white counterpart, brown fat acts as a natural defense against both cold temperatures and obesity, by burning energy using its higher levels of mitochondria. Brown fat is also often located in hard to reach places in the body, and leveraging its energy-burning capabilities isn't easy.
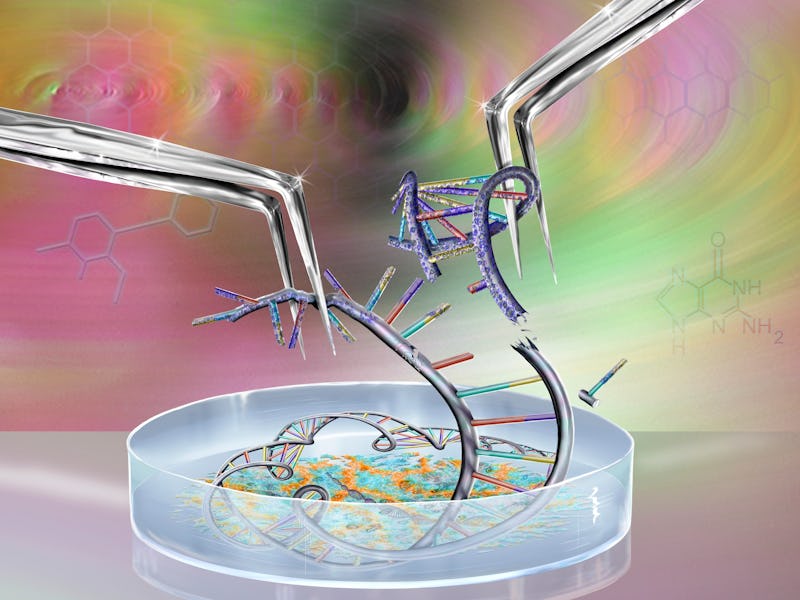
In the study, researchers harnessed CRISPR — a type of gene-editing technology that enables scientists to edit DNA sequences — to endow white fat with brown fat's energy-burning properties.
Using CRISPR, the team activated human white fat cells to express higher amounts of uncoupling protein 1 (UCP1), which drives the burning of fat in brown fat tissue. In turn, these white fat cells became brown-like cells (HUMBLE).
After engineering these HUMBLE cells, the team transplanted them into obese mice and monitored their response over 12 weeks.
Animals that received HUMBLE cell transplants showed an uptick in energy expenditure and insulin sensitivity, two markers that indicate improved metabolic health. They also gained less weight and had smaller droplets of fat in their fat tissue.
HUMBLE cells appear to activate brown fat tissue by boosting the production of the chemical nitric oxide, which helps regulate energy metabolism.
Mitochondria in the engineered HUMBLE cells were more similar to mitochondria in brown fat cells than in white fat cells.
What's next? — Obesity isn't just carrying extra weight. It can cause a cascade of negative health effects like heart disease, stroke, type 2 diabetes, and certain types of cancer. As most adult humans know, losing weight to stave off these nasty side effects is a lot more complicated than it sounds.
But many more experiments — in humans, not mice — need to be conducted before we can say we've got a beneficial intervention.
Tseng stresses that even if the new CRISPR cell therapy does make its way into clinical practice, health providers should still encourage lifestyle interventions like changing diet and exercising before trying the treatment.
However, there are certain individuals that are either genetically predisposed to obesity, have physical difficulty in exercising, or who have already developed the disease and the complications related to it. This group needs to be "immediately treated," Tseng says.
"That's what we hope this therapeutic approach can help with."
Current treatments for obesity, like bariatric surgery or weight loss medications, are risky and relatively invasive, Tseng says. This cell therapy, if proven effective, could offer a cheaper, safer, and less invasive technique to fight obesity. She predicts that this approach could possibly be applied in a few years.
"The procedure is going to become easier and the cost is going to be reduced, so it may become a more routine procedure in the future," she predicts.
"Treating obesity is one of the major challenges currently in the medical field."
Abstract: Brown and brown-like beige/brite adipocytes dissipate energy and have been proposed as therapeutic targets to combat metabolic disorders. However, the therapeutic effects of cell-based therapy in humans remain unclear. Here, we created human brown-like (HUMBLE) cells by engineering human white preadipocytes using CRISPR-Cas9– SAM–gRNA to activate endogenous uncoupling protein 1 expression. Obese mice that received HUMBLE cell trans- plants showed a sustained improvement in glucose tolerance and insulin sensitivity, as well as increased energy expenditure. Mechanistically, increased arginine/nitric oxide (NO) metabolism in HUMBLE adipocytes promoted the production of NO that was carried by S-nitrosothiols and nitrite in red blood cells to activate endogenous brown fat and improved glucose homeostasis in recipient animals. Together, these data demonstrate the utility of using CRISPR-Cas9 technology to engineer human white adipocytes to display brown fat-like phenotypes and may open up cell-based therapeutic opportunities to combat obesity and diabetes.
This article was originally published on