Brain study debunks a common explanation for what causes a 'broken heart'
Thirty percent of patients don’t experience what’s typically considered the cause.
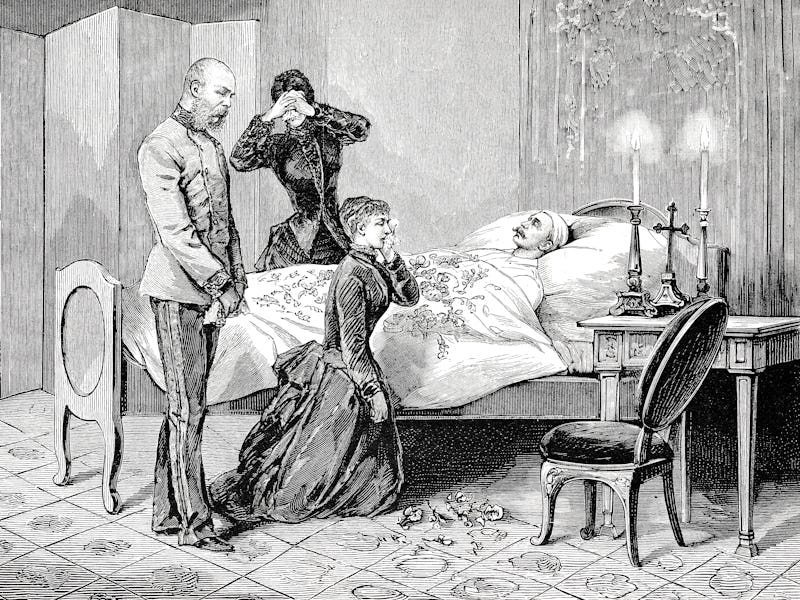
It sounds like something you’d find in Shakespeare, but you can actually die of a broken heart.
Takotsubo syndrome (TSS), also known as “broken heart syndrome,” is stress-induced cardiomyopathy. This means a sudden, usually temporary, weakening of the heart muscles.
It’s thought to occur after a significant, once-in-a-lifetime stressful event, like the death of a spouse. But that part is a bit mysterious, considering about 30 percent of patients with the syndrome have no identifiable trigger event.
Now, researchers from Massachusetts General Hospital and Harvard Medical School may have solved at least one part of the riddle. Their findings, published Friday in the journal European Society of Cardiology, may fundamentally change our understanding of how the syndrome works.
The background — It’s known that activity in the amygdala, also known as the “stress portion” of the brain can predispose people to heart attacks. People with TSS and people without TSS also display different levels of brain activity, especially around the amygdala
Co-author Ahmed Tawakol is the co-director of the Cardiovascular Imaging Research Center at Massachusetts General Hospital and Harvard Medical School.
“We know the brains of people with TSS have more activity in areas associated with stress,” Tawakol tells Inverse. “But it wasn't clear if it was the result of the syndrome, or maybe a cause of it. And that’s what we wanted to find out.”
Tawakol and his team retrospectively identified the positron emission tomography (PET) scans of 41 people who had developed TSS sometime after their initial scans. They then examined a control group — people who matched the individuals in the TSS group in age, sex, ethnicity, and health, minus having TSS. They had the control undergo PET scans and then compared the two.
What they discovered, Tawakol says, was “very surprising.”
The link between stress and heart attacks
Before getting into exactly what they found, it’s important to understand the connection between stress and heart attacks. When you’re stressed, your sympathetic nervous system is activated–-you’re going into fight-or-flight mode. Adrenaline and other hormones are released, raising your blood pressure. Making matters worse, is how your immune system responds.
When you’re stressed, Tawakol says, “Sympathetic nervous system fibers go into your bone marrow, in addition to a bunch of other places. In the bone marrow, it stimulates the production of immune cells.” Unfortunately, it stimulates pro-inflammatory immune cells, like cytokines. Chronic stress can, in turn, lead to chronic inflammation.
Digging into the details — When comparing the PET scans, the researchers were particularly concerned with how well the amygdala and prefrontal cortex communicated. The amygdala is often referred to as part of our “lizard brain” — it’s involved in those immediate, unthinking fight or flight responses. The prefrontal cortex is where our executive functioning happens, including our ability to contextualize the triggers our amygdala perceives as threats.
“If you hear someone slam a door outside your house, your amygdala will register very quickly,” Tawakol explains.
“If it had its own way, it will continue to run with it and say, is that an accident? Am I in danger? Is there an explosion? Was that a gunshot?”
The researchers were particularly concerned with how well the amygdala and prefrontal cortex communicated.
The prefrontal cortex, meanwhile, contextualizes what’s happening for the amygdala. If it’s just a routine slamming door that the brain has heard millions of times, it will tell the amygdala to chill out. That’s why communication between the two is so important.
Without proper communication, the amygdala is like your friend who ate a too strong edible and thinks everyone in the movie theater is staring at him. Your prefrontal cortex is the sober friend who reminds him that they’re sitting in the front row of a movie theater and everyone is actually looking at the screen.
When the researchers compared the scans between the TSS and control group, they evaluated the ratio of activity in the amygdala to the prefrontal cortex/regulatory activity. The people with TSS had a much higher ratio of amygdalar activity to regulatory activity. In the control group, the ratio was much more balanced.
That supported the researchers’ hypothesis. But the comparison showed something else–-something that was completely unexpected.
What they discovered — When the researchers looked at the TSS group, they noticed something interesting about when different individuals in the group developed TSS.
“If [TSS] is triggered by something like the death of a spouse, your amygdalar levels shouldn’t make a difference,” Tawakol says, “They might make you more or less susceptible to developing it upon exposure to that external trigger. But it's not going to impact the timing.”
But what the researchers actually found is that it did associate with the timing. The people with the highest rates of amygdalar activity developed TSS about two years faster than individuals with lower amygdala activity
The researchers don’t know exactly why that is, but Tawakol has a hypothesis: It may not be just the one stressor that matters, but the combination of stressors, and how the brain is primed to react to stress.
“You could imagine that the more triggered your brain is by stress, the lower the threshold is for you to develop this syndrome and other stress-related disorders,” he explains. It might not be triggered by a once-in-a-lifetime stressor, but something relatively mild.
Why this matters — This may explain why one-third of people who develop the syndrome don’t have a significant stressor to point to as the cause.
“If you have a very, very hyperactive amygdala, then [developing TSS] might take a lesser insult,” he says. “And that insult can come anytime, the next time in your routine colonoscopy, even.”
That may sound scary if you, like many people, are often stressed. However, Tawakol says not to worry: The wiring that makes us so prone to stress is malleable.
Meanwhile, “a bunch of activities can change that wiring,” Tawakol says. Healthy lifestyle behaviors like good sleep and exercise can help mitigate stress, and all the terrible things it does to our body.
“If you think of the amygdala, like a muscle, it's something that you can build up or shrink,” he says. “And the same is said in the opposite direction for the prefrontal cortex. So a lot of those healthy lifestyle behaviors actually make the prefrontal cortex more robust.” A more robust prefrontal cortex means a more restrained amygdala.
No one can avoid getting their heart broken. But if we can reduce our stress levels, we may be able to avoid getting broken heart syndrome.
Abstract:
Aims: Activity in the amygdala, a brain centre involved in the perception of and response to stressors, associates with: (i) heightened sympathetic nervous system and inflammatory output and (ii) risk of cardiovascular disease. We hypothesized that the amygdalar activity (AmygA) ratio is heightened among individuals who develop Takotsubo syndrome (TTS), a heart failure syndrome often triggered by acute stress. We tested the hypotheses that (i) heightened AmygA precedes development of TTS and (ii) those with the highest AmygA develop the syndrome earliest.
Methods and results: Individuals (N=104, median age 67.5 years, 72% female, 86% with malignancy) who underwent clinical 18 F-FDG-PET/CT imaging were retrospectively identified: 41 who subsequently developed TTS and 63 matched controls (median follow-up 2.5 years after imaging). AmygA was measured using validated methods. Individuals with (vs. without) subsequent TTS had higher baseline AmygA (P=0.038) after adjusting for TTS risk factors. Further, AmygA associated with the risk for subsequent TTS after adjustment for risk factors [standardized hazard ratio (95% confidence interval): 1.643 (1.189, 2.270), P=0.003]. Among the subset of individuals who developed TTS, those with the highest AmygA (>mean + 1 SD) developed TTS ∼2 years earlier after imaging vs. those with lower AmygA (P=0.028).
Conclusion: Higher AmygA associates with an increased risk for TTS among a retrospective population with a high rate of malignancy. This heightened neurobiological activity is present years before the onset of TTS and may impact the timing of the syndrome. Accordingly, heightened stress-associated neural activity may represent a therapeutic target to reduce stress-related diseases, including TTS.
This article was originally published on