This Party Drug Completely Restructures The Brain's Dopamine System, Scientists Find
Prolonged ketamine exposure switches up the brain’s dopamine system in ways that could help people struggling with a variety of mental health issues.
Our brains are not static objects — they adapt and reorganize to the ebb and flow of new information, sensations, and even physical trauma. But when this impressive neuroplasticity is impaired, it can cause psychiatric disorders like major depression and schizophrenia. To help heal these mental maladies, scientists are turning to a formerly illicit drug to help rewire — and ultimately heal — the brain.
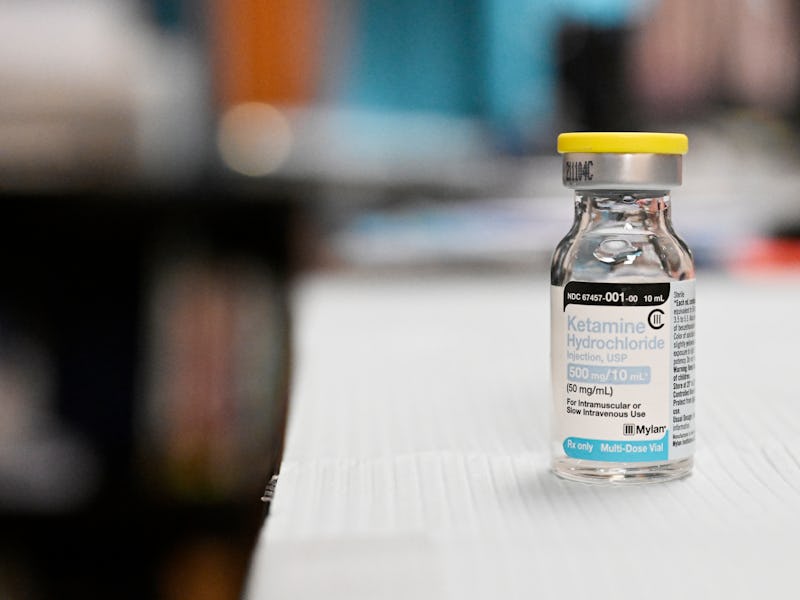
There’s no shortage of research extolling ketamine’s power in improving mental health, bringing the drug increasingly mainstream with ketamine clinics and teletherapies, as well as federally approved treatments. Now, a new study seeks to understand how exactly ketamine works in the brain when it’s used for a long time and map out where it switches up neural connectivity.
Published earlier this month in the journal Cell Reports, researchers at Columbia University performed high-resolution brain imaging on mice that were given ketamine repeatedly over differing timescales, including one, five, and 10 days. It was after this final, 10-day threshold that scientists saw widespread structural changes in the brain’s dopamine system, (aka the “feel good” neurotransmitter). The researchers say this finding calls for more targeted ketamine therapies that take into consideration the condition being treated and the brain area involved instead of a blanket, “one size fits all” approach.
“Instead of bathing the entire brain in ketamine, as most therapies now do, our whole-brain mapping data indicates that a safer approach would be to target specific parts of the brain with it, so as to minimize unintended effects on other dopamine regions of the brain,” Raju Tomer, an assistant professor of biological sciences at Columbia University who led the study, said in a press release.
Revamping dopamine
In the study, Tomer and his colleagues had two groups of male mice, one repeatedly injected with a dose of ketamine equivalent to what’s given to mice genetically engineered to have depression, and the other an anesthesia-inducing dose (ketamine is also used as an anesthetic). A third group of control mice were given plain saline.
The researchers found that there was a measurable change in the dopamine-releasing neurons after 10 days at both doses. Drilling down to specific parts of the mousy brain, there was an uptick in these neurons in the hypothalamus, which is responsible for regulating the body’s metabolism and maintaining homeostasis. But in areas linked to regulating mood, like the midbrain, there was a drop in dopamine neurons.
It was not only the amount of dopamine neurons but changes in pathways involving dopamine between different brain regions. There was an increase in connections to the prefrontal cortex, which is involved in higher-order cognitive functions. On the flip side, there were decreases in the pathways to the sensory, visual, and auditory cortex. This latter finding, in particular, could explain the distortions in sight and sound perception, as well as the dissociative effects users on ketamine experience while on the drug.
“The restructuring of the brain’s dopamine system that we see after repeated ketamine use may be linked to cognitive behavioral changes over time,” Malika Datta, a co-author of the study and formerly of Columbia University, said in the press release.
The researchers say this is the first time the subcellular mapping of ketamine’s effect on the whole brain has been attempted, as previous studies have largely been hypothesis-driven with a focus on specific areas of the brain. However, these findings are only in mice and need further validation in future studies to truly understand ketamine’s long-term effects on humans.
However, the new study does set a precedent for strongly considering optimizing therapeutic ketamine with a delivery system targeting a specific part of the brain. The findings may also illuminate why ketamine helps treat a wide range of medical conditions, such as alcoholism and eating disorders, and a better understanding of why its overuse can run the risk of schizophrenia-like symptoms.
“This study gives us a deeper brain-wide perspective of how ketamine functions that we hope will contribute to improved uses of this highly promising drug in various clinical settings as well as help minimize its recreational abuse,” Tomer said. ”More broadly, the study demonstrates that the same type of neurons located in different brain regions can be affected differently by the same drug.”