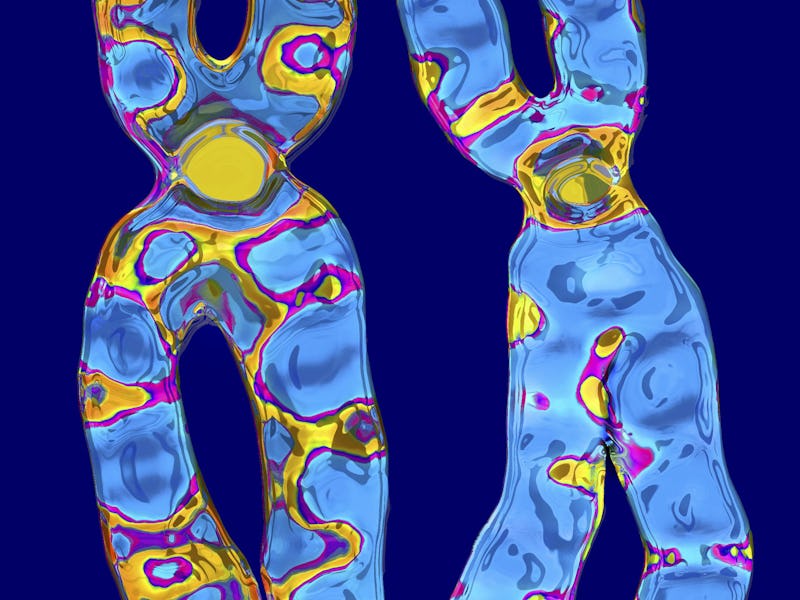
This Chromosome Could Reveal Why Women Get Way More Autoimmune Diseases Than Men
X chromosome inactivation is a crucial biological process with some inadvertent autoimmune consequences.
Shaped by thousands of years of evolution, the body’s immune system is a vigilant guardian primed against external infectious threats. Too much vigilance, however, and this guardian of potent cells and chemicals instead becomes our own adversary. The result is a myriad of autoimmune diseases affecting around one in five Americans and around four percent worldwide.
While one’s risk for autoimmune disease is partly genetic, individuals who are disproportionately affected tend to be those assigned female at birth — a shocking 78 percent. Why there’s such a staggering difference has been a mystery, but scientists have been narrowing down suspects to risk factors like hormones, the gut microbiome, and now, the X chromosome itself.
Researchers led by Stanford University found that a routine biological process that silences one X chromosome in females (called X chromosome inactivation) may be a risk factor for autoimmune diseases. In particular, proteins that help with the silencing process might seem foreign to our bodies, and the body might create antibodies against them, setting the stage for autoimmune diseases.
When male mice prone to autoimmune disease were genetically engineered with the Xist gene, they also showed signs of autoimmunity similar to what’s seen in their female counterparts. In blood samples collected from human participants with autoimmune diseases, the researchers also found antibodies against the proteins involved in X chromosome inactivation.
These findings were published Thursday in the journal Cell.
“Scientists have a better idea now of pinpointing the autoimmune risk associated in different sexes, and this comes from the chromosomal basis, individual molecules we can now perhaps pin this [to],” Howard Chang, professor of cancer research and genetics at Stanford University of Medicine, who led the study, tells Inverse.
The master silencer
All humans and many other mammals have a pair of sex chromosomes: two Xs for biological females and one X and one Y for biological males. Because chromosomes are basically individual recipe books that a cell uses whenever it needs to make something, having duplicates of the same book means the cell would end up making more than it needs, like making twice as many cakes. Twice as many cakes may sound benign, but for a cell, having that many genes turned on and baking all their proteins and other molecules they code for would be lethal.
To balance out the books, each cell randomly chooses an X chromosome to muffle during early embryonic development. As you might guess, this doesn’t happen in biological males, as they only have one X chromosome.
This biological silencing is handled by a gene found on the X chromosome called Xist, which was first discovered in the early 1990s. Xist doesn’t code for any protein — almost 99 percent of DNA doesn’t; instead, this gene manufactures something called long noncoding RNA, RNA being a Xerox copy of DNA that’s free to float around in the cell, unlike DNA packed away in chromosomes and confined to the nucleus.
Paradoxically, Xist is turned on in whichever X chromosome gets the short stick, says Chang. Its long noncoding RNA recruits other proteins to join in on the silencing, the whole mass of RNA and proteins sticking together to form what scientists call a ribonucleoprotein complex. This complex then coats the X chromosome like some sort of form-fitting molecular bodysuit.
In 2015, Chang and a group of other researchers published a paper cataloging the proteins forming the ribonucleoprotein complex. They didn’t have autoimmune disease on their minds, per se, when conducting their study but discovered many of the proteins associated with the complex could become parts of autoantibodies, aka antibodies that respond to and attack your own cells and tissues.
This discovery had the researchers wondering: Is Xist, the master silencer, somehow nefariously involved in autoimmune disease?
Genetics + environment
To answer that question, Chang and his colleagues inserted the Xist gene into the genome of male mice, some of whom were susceptible to autoimmune disease and others resistant. The Xist gene was tweaked so it could be turned on and off at will by chemical means, and the portion of the gene that instructs its RNA to silence the X chromosome was deleted. However, the long noncoding RNA could still mingle with other proteins to make its ribonucleoprotein complex. The experiment also included male mice where Xist wasn’t turned on, female mice, and healthy, otherwise normal mice.
Turning on Xist itself didn’t trigger autoimmunity, but when the mice were injected with pristane, a compound known to cause a lupus-like disease in the animals, that’s where Chang and his colleagues noticed signs of autoimmune disease in the genetically vulnerable mice on par with some of the female mice injected with pristane.
“Because we made a male mouse get [autoimmune] disease just with this RNA, that really shows that you don’t need female hormones,” says Chang. “You don’t even need a second X chromosome, just this RNA can confer a lot of the risk.”
In mice with Xist who weren’t susceptible to autoimmune disease, nothing really happened to them, which Chang says highlights how not just Xist alone but one’s genetic susceptibility for conditions like lupus, inflammatory bowel disease, or multiple sclerosis (and exposures to potential environmental triggers) needs to be present to explain one’s risk for autoimmune disease.
These findings are just the first step in unraveling the complexity of autoimmune disease and identifying more precise diagnostics and treatments to better help patients, says Chang. However, there are some limitations, namely the fact this study was in mice using an engineered form of Xist, not the one normally found in the X chromosome.
“If you use a version [of Xist] that’s slightly different, that could lead to slightly different results,” he says.
In a separate but parallel study, the researcher analyzed blood samples obtained from anonymous donations to the Stanford Blood Center. In those whose blood demonstrated signs of autoimmunity with autoantibodies, those antibodies were reactive to 79 out of the 81 proteins part of Xist’s ribonucleoprotein complex. So there is a basis for Xist potentially mediating autoimmune disease in humans, although Chang says he would love to see these results replicated in a larger population.
For upcoming studies, the researchers would also like to suss out how exactly the immune system chances upon this ribonucleoprotein complex since it's otherwise sequestered inside the cell's nucleus, out of sight by immune cells.
“Understanding what different triggers do, whether they cause cell death in a way that leaks out small or large amounts of Xist, that would be a useful thing to think about in the future,” says Chang.