The Trick That Kept Our Ancestors From Starving May Contribute to Obesity
It's an "anti-starvation mechanism that has become a curse in times of plenty."
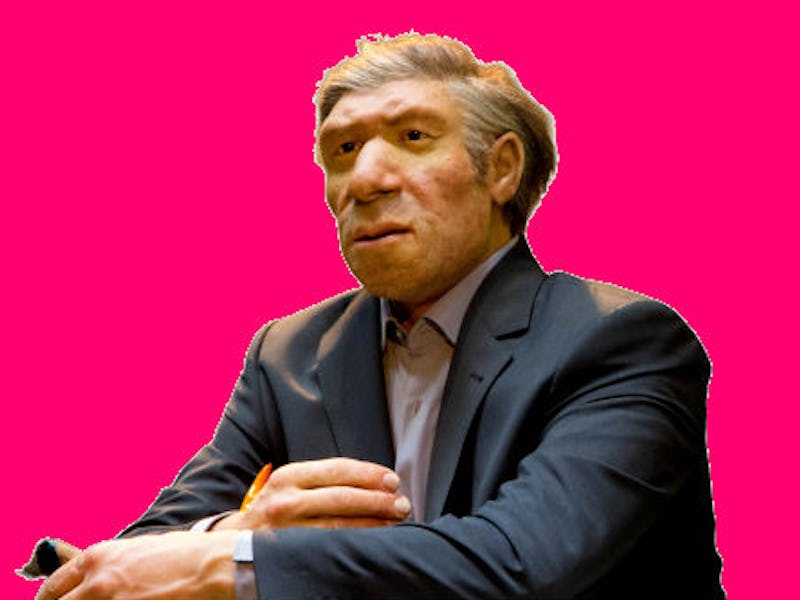
Early humans had to hang on to every last ounce of energy if they wanted to have any hope for survival. As a result, over the course of thousands of years, our bodies got a bit too good at latching onto fat, a skill that’s become a burden now that food is plentiful. Now scientists believe they’ve figured out one way our bodies have adapted to storing fat over all those years, and they hope that one day we will find a way to control it.
In a paper published Tuesday in Cell Reports, a team of scientists at New York University School of Medicine notes that a protein called RAGE seems to control how the body expends energy. Corresponding author Ann Marie Schmidt, M.D., describes RAGE — which stands for “receptor for advanced glycation end products” — as a cellular “brake” on fat burning.
In a series of mouse experiments, Schmidt’s team showed that RAGE may be a survival tool gone awry, and it could be contributing to obesity.
Schmidt proposes that the RAGE proteins can control the way the body burns through fat stores.
To get a sense of how RAGE keeps fat burning in check, Schmidt and her colleagues genetically manipulated mice to not express that RAGE protein. In these mice, genes related to maintaining body temperature tended to become more active. That, the team says, demonstrates that these mice’s bodies were just working a bit harder at rest.
As a consequence, the mice lost weight. Even during a regimen of high-fat feeding, mice without RAGE gained significantly less weight than those with the RAGE protein. And when they transplanted fat cells containing RAGE into the mice who had initially had the protein knocked out, the mice started gaining weight again.
Does this mean that the key to increasing fat burning would be to remove the protein in humans too? Probably not, considering that in our history, this protein was probably our key to survival when food was scarce, and burning through fuel at higher rates was more of a liability than an asset. But the key is figuring out what circumstances tend to make RAGE more active than it already is.
RAGE binds to a class of molecules called advanced glycation end products or AGEs. As these authors note, the molecules that bind to RAGE are often released during times of metabolic stress, like during extreme cold or starvation periods.
That, they write, suggests that RAGE isn’t typically activated during times of homeostasis (when things are all going according to plan) but rather, when things are going wrong. And Schmidt notes that she believes overeating may be a scenario in which these proteins are activated.
“We discovered an anti-starvation mechanism that has become a curse in times of plenty because it sees cellular stress created by overeating as similar to stress created by starvation — and puts the brakes on our ability to burn fat,” she said in a statement.
Overeating is a contributor to obesity all on its own, and there are plenty of explanations hidden in the brain and the body that help explain our drive to consume more than we need. But Schmidt’s idea suggests that overconsumption itself may trigger a deep seated cellular response that tells our body to expect tough times ahead.
Schmidt’s team’s next challenge will be to see whether there are ways to safely manipulate that pathway, which has served us so well throughout human history but is causing more harm than good these days.
Abstract: Exquisite regulation of energy homeostasis protects from nutrient deprivation but causes metabolic dysfunction upon nutrient excess. In human and murine adipose tissue, the accumulation of ligands of the receptor for advanced glycation end products (RAGE) accompanies obesity, implicating this receptor in energy metabolism. Here, we demonstrate that mice bearing global- or adipocyte-specific deletion of Ager, the gene encoding RAGE, display superior metabolic recovery after fasting, a cold challenge, or high-fat feeding. The RAGE-dependent mechanisms were traced to suppression of protein kinase A (PKA)-mediated phosphorylation of its key targets, hormone-sensitive lipase and p38 mitogen-activated protein kinase, upon β-adrenergic receptor stimulation—processes that dampen the expression and activity of uncoupling protein 1 (UCP1) and thermogenic programs. This work identifies the innate role of the RAGE as a key node in the immunometabolic networks that control responses to nutrient supply and cold challenges, and it unveils opportunities to harness energy expenditure in environmental and metabolic stress.