Could We Get a Universal Flu Vaccine?
New research says we’re one step closer.
Every year, seasonal influenza infects five to 20 percent of the U.S. population, and results in 200,000 hospitalizations. That includes 36,000 deaths from flu-related complications. And the best way to protect yourself is to get vaccinated.
The problem with the flu vaccine, however, is that it varies every year. The flu virus is constantly mutating. Public health officials and epidemiologists have to predict which strains are likely to cause the most infections, and many times the process requires a lot of guesswork. That’s why it comes as no surprise when the vaccine only reduces risks caused by flu by a meager rate — such as 23 percent last year.
But scientists might be a bit closer to developing a vaccine that could potentially protect against the entire family of influenza virus strains. Two groups of researchers — from the National Instutites of Health, and the Crucell Vaccine Institute — are reporting their findings today in the journals Nature Medicine and Science, detailing how they’ve transformed a piece of flu virus protein to protect against a whole slew of flu strains.
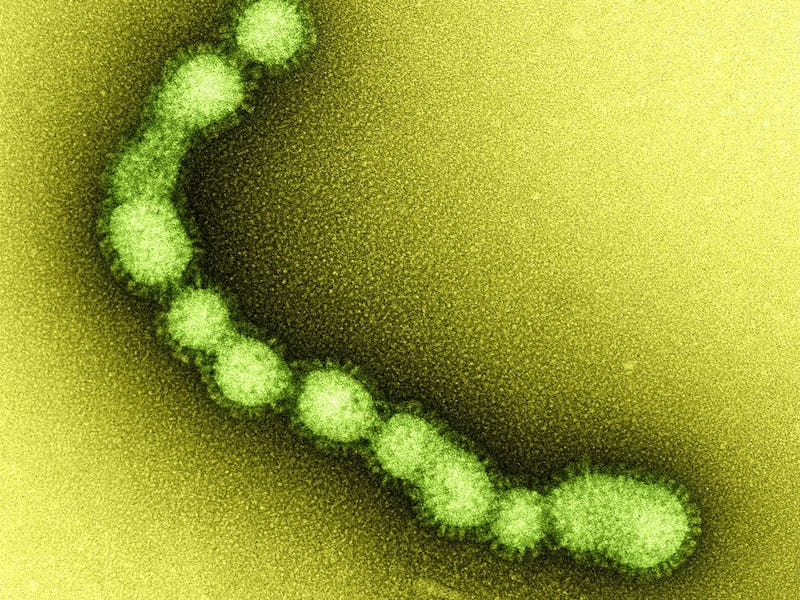
Flu viruses come and go as they please while being covered in a protein called hemagglutinin (or HA), which allows them to sneak into healthy host cells. Human immune systems produce antibodies to neutralize the heads of HAs. Unfortunately, HAs tend to mutate rapidly and ensure that previously-made antibodies are unable to work against successor flu strains.
However, the stems of HAs tend to stay the same. Therein lies the potential: If you could make a vaccine that spurs an immune system to protect against the stem, it could help protect against at least a huge segment of flu viruses.
The problem is that the immune system doesn’t really target stems. Gary Nabel, who oversaw one of the studies as former head of the NIH’s Vaccine Research Center, told Wired it’s similar to how the the branches and leaves of trees are the most visible from overhead, and you have to chop them off to see the trunk. HAs are the same way — which is why the immune system targets the head first. And without heads, the HAs tend to fall apart too fast for antibodies to bind to them.
The NIH team decided to work on bacteria-derived nanoparticles that attach to the HA stem and hold it together so it triggers an immune response; the Crucell Vaccine Center researchers changed the amino acid structure in a headless mini-HA structure to keep it stable.
Vaccines made from these materials were able to protect mice against H5N1 flu, and also confer partial protection against other related strains. The nanoparticles also protected four of six ferrets from avian flu, while the mini-HA vaccine helped reduce fevers in five swine-flu infected monkeys.
All of this is just preliminary work — a lot more testing will be needed before this can be a realistic way to protect humans from the flu. But it’s a big step forward that could pave the way to a universal flu vaccine, and perhaps even point to how we can go about making vaccines for other viruses that mutate rapidly, like HIV or the common cold.