Psychedelic Drugs Reshape Cells to "Repair" Neurons in Our Brains
Psychedelics could show the way to a new generation of medicine.
Psychedelic drugs like LSD, DMT, and psilocybin (the chemical in magic mushrooms) have shaken off a lot of their stigma and reputation as party drugs in the past few years, as scientists begin to investigate their significant healing potential for people with mental illness. Similarly, the drug ketamine, best known as a rave drug, has also shown promise in rapidly treating medication-resistant depression, and like psychedelics, its effects persist after treatment has ended.
New research shows that the way psychedelics repair the brain is very similar to ketamine’s action, which could pave the way for a future class of fast-acting drugs to treat conditions like depression, post-traumatic stress disorder, and substance use disorders. In a paper published Tuesday in the journal Cell Reports, a team of researchers showed evidence that psychedelic drugs can induce structural changes in nerve cells — a trait called neuroplasticity — that could, in turn, help repair brain dysfunction in people with mood and anxiety disorders.
“Psychedelics are some of the most powerful compounds known to impact brain function so I was very interested to know what their mechanisms of action are,” David Olson, Ph.D., an assistant professor of biochemistry and molecular medicine at UC Davis and the corresponding author on the study, tells Inverse. This paper adds to the on growing body of psychedelic neuroscience research by showing some of the changes induced by psychedelics.
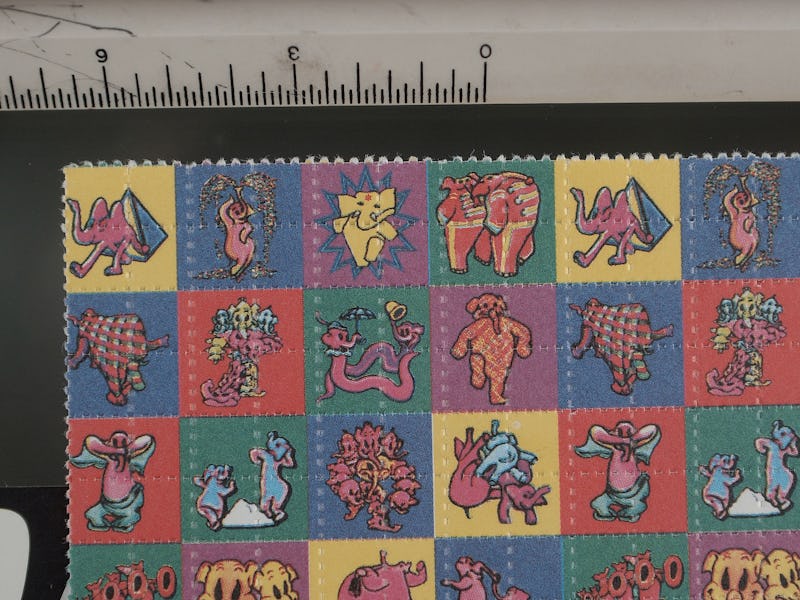
An untreated neuron (blue) shows fewer dendrites (branches) than the one treated with LSD.
Through experiments conducted on cultured rat neurons, as well as the actual brains of fruit flies and rats, Olson and his colleagues found that LSD, DMT, and DOI (2,5-dimethoxy-4-iodoamphetamine, a potent psychedelic amphetamine) increased the number of dendrites (branches) in nerve cells, increased the density of dendritic spines (protrusions on dendrites that help the neurons receive input from other cells), and increased number of synapses (functional connections between neurons). Altogether, these findings suggest that psychedelics induce structural changes to the brain, which Olson says can help treat mental illness.
“The structure of neurons affects their function, and in the case of a lot of neuropsychiatric diseases, particularly mood and anxiety disorders, these are characterized by an atrophy of neurons in the prefrontal cortex, a key brain region that regulates emotion, fear, and reward,” says Olson. “So if we can find compounds that promote growth of those neurons we might be able to repair the circuits are damaged in those diseases.”
Since prefrontal cortex helps control other areas of the brain involved in fear, anxiety, and reward, says Olson, it’s a critical region for the treatment of depression, PTSD, and substance use disorders.
Crystalline DMT is often vaporized in small amounts (2-60 milligrams) out of a glass bulb-style pipe. Researchers have found that DMT changes the structure of neurons, hinting at the mechanism for its mental health benefits.
But Olson and his co-authors aren’t just interested in using psychedelics to treat patients. They hope to use psychedelic compounds as tools to dig down into the biochemical signaling pathways that lead to the neuroplasticity observed in this study. By identifying the specific ways in which psychedelics act on the nervous system, Olson and his colleagues hope that they can develop a new generation of drugs that will replicate — or improve upon — the rapid, long-lasting healing effects of ketamine and psychedelics, but without the potential for abuse or challenging experiences.
“That’s the ultimate goal: to use psychedelics as inspiration for better medicine,” Olson says.
Of course, this is just one snapshot of the neuronal changes induced by psychedelics, so further research will be necessary to find out long-term effects on brain function.
“Plasticity is not universally a good thing. We were hoping to induce plasticity in prefrontal cortex, which can be potentially useful for treating mood and anxiety disorders, but promoting plasticity in other parts of the brain, like the amygdala can induce anxiety,” says Olson. “It’s very unclear what the risks are right now.”