1 in 9 Men Now Have Oral HPV: What Does That Mean For You?
The STI is more and more becoming a men's problem.
Oral human papillomavirus infections are on the rise among men. This is not a good thing, as HPV is associated with several different kinds of cancer. And since this trend doesn’t appear to be going away, it’s time for men to get educated about what having HPV — or being at risk of having HPV — really means.
In a study published in the journal Annals of Internal Medicine and funded by the National Cancer Institute, researchers examined data from 4,493 men and 4,641 women between the ages of 18 and 69, and they found that 11.5 percent of men tested for HPV had oral HPV (the term for when the virus is found in the mouth and throat), compared to just 3.2 percent of women.
Beyond the fact that HPV can cause unwelcome — but treatable — warts on a person’s genitals, mouth, and anus, some types of HPV can also cause a number of cancers. Researchers found men are much more likely than women to carry high-risk forms of HPV, the types more likely to cause cancer — 7.3 percent versus just 1.4 for women. There are over 100 types of HPV, of which at least 13 have been discovered to be cancer-causing.
Researchers say oral HPV is on the rise among men. The solution? "Use protection. Get vaccinated."
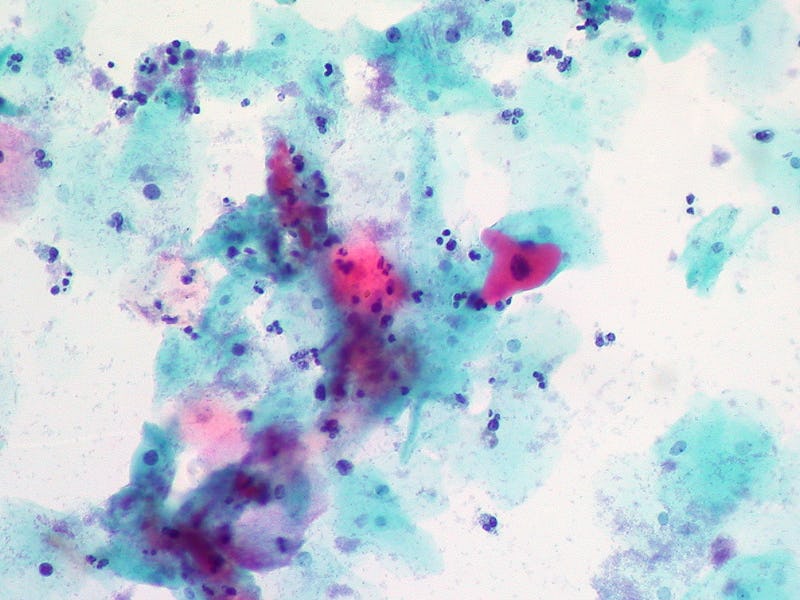
One of the most common types of cancer caused by oral HPV is oropharyngeal squamous cell carcinoma (OPSCC). This type of throat cancer occurs in about 50,000 people a year, and according to the study’s authors, it’s on the rise among men.
“Traditionally HPV infection was considered a problem among women; however, a growing body of knowledge — including our findings — show that oral and genital HPV infection prevalence and concordance of oral-genital HPV is disproportionately high among men,” Dr. Ashish Deshmukh, one of the study’s authors, tells Inverse.
Deshmukh, a research assistant professor in the Department of Health Services Research, Management and Policy at the University of Florida, says HPV-related cancer rates have fallen for women but risen for men. He says OPSCC rates among men have risen more than 250 percent over the last 20 to 30 years while the rates for women have remained constant or declined.
“Recent rates show that oropharyngeal cancer among men has already surpassed cervical cancer, and OPSCC is now the most common HPV-related cancer in the U.S.,” he says.
But let’s get back to the question of what can be done about this.
Deshmukh says the advice is pretty similar to what you’d hear for any other sexually transmitted infection: “Use protection. Get vaccinated.” Unfortunately, HPV is different from many other sexually transmitted infections in that there is no test for men. There is, however, a vaccine, but research shows that it’s drastically underused among young men.
Regarding cancer risks, Deshmukh says there is not a lot to do unless you’re an individual who may be at a higher risk for HPV.
“No cancer screening recommendations exist among men,” he says. “However, it is essential for high-risk individuals, for example, HIV-positive men and men who have sex with men, to get screened for anal cancer (another HPV-related cancer). There are no national anal cancer screening recommendations, but NY State Department of AIDS Institute recommends screening these individuals.”
Regarding vaccinations, there’s no clear evidence of how vaccines affect people once they’re already infected. If you’re young and only beginning to be sexually active it could definitely be worth talking to your doctor about getting the vaccine. And we might see more evidence down the road that the vaccine can help people who already have HPV.
It may not be entirely reassuring to know that there’s not much you can do if you already have HPV, but many types of HPV are low-risk. And additionally, you can still minimize the risk of transmission for yourself or your partner by always using male (or female) condoms.