Researchers Develop a Test for Depression and Schizophrenia
This is a big step forward in the search for physical diagnoses.
Researchers have zeroed in on a key biological receptor to test for depression and schizophrenia — even before symptoms appear. It’s a promising first step to identifying subtypes of both diseases, for which there are currently no physical diagnostic tests.
For some manifestations of depression and schizophrenia, the root is a receptor known as Altered N-methyl-D-aspartate, or NMDAR. The signaling of that receptor appears to be increased for some patients with depression, but decreased for some with schizophrenia. By manipulating NMDAR — either blocking or stimulating it — we can extrapolate from the patient’s reaction whether they’re vulnerable to either disease. The research was published Monday in the journal Experimental Physiology.
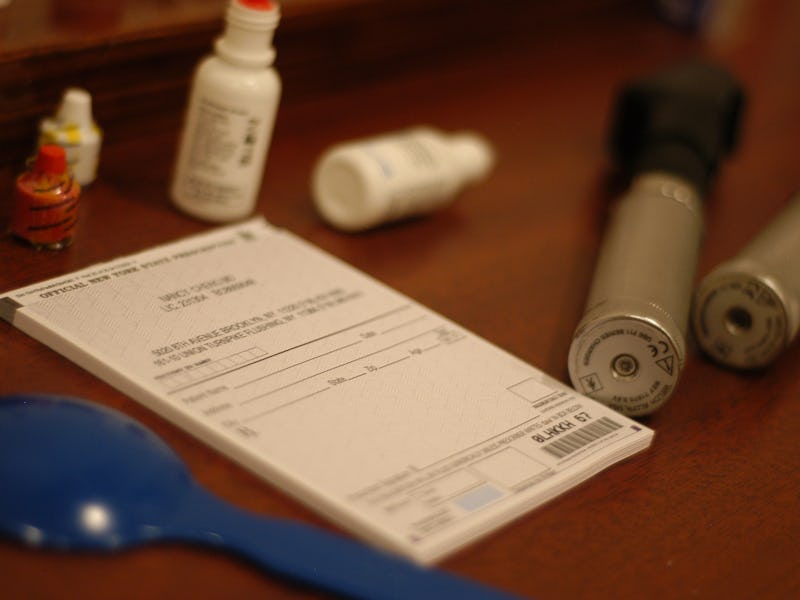
The test works via an infusion component called hypertonic saline, which increases salt concentration in the blood. Infusion lasts for two hours; blood is collected perhaps a dozen times and measured over time for the slope of the reaction the researchers are looking to trigger — release of a hormone called arginine-vasopressin, or AVP.
“Now, why I’m interested in AVP is because release of it from the brain is directly linked to the NMDA receptor,” co-author Handan Gunduz-Bruce tells Inverse. “Our hypothesis here is that while in depression you think the receptor is working too much we should see a high slope, and in schizophrenia if it’s not functioning too well we should see a low slope.”
While her resources are limited at the moment, the research has already yielded very high responses in certain subgroups of depression and very low ones in subgroups of schizophrenia. The caveat with this research is to approach it not as a definitive mental-health test — there’s still nothing that is — but as a vulnerability marker. In other words, we have tens of thousands of genes, and with them individual vulnerabilities toward certain illnesses over others.
This research won’t benefit everyone with depression or schizophrenia, because there are subtypes of each disease that don’t owe their mechanism of action to the NMDA receptor. But it could be a lifesaver for the people with the types that do — leading to earlier diagnoses, better treatment, and better understanding of their own psychology.
“If we can detect these,” Gunduz-Bruce says, “I think we have a big advantage. There’s more work to be done, but if we get the grants, the funding we need … it might be within the next five years.”
Abstract
Altered N-methyl-D-aspartate (NMDA) receptor activity and glutamate signaling may underlie the pathogenesis of both schizophrenia and depression in subgroups of patients. In schizophrenia, pharmacologic modeling, postmortem and imaging data suggest reduced NMDA signaling. In contrast, recent clinical trials demonstrating the efficacy of the NMDA antagonist ketamine in severely depressed patients suggest increased NMDA receptor signaling. We conducted a proof of concept study to assess whether there is any in vivo evidence for an inverse association in depression and schizophrenia with respect to the NMDA receptor function. For this purpose we used a translational approach, based on findings from animal studies that NMDA receptor is a key mediator of arginine-vasopressin (AVP) release into the bloodstream. Using hypertonic saline to induce AVP release, as done in animal studies, we found that in depressed patients, NMDA receptor mediated AVP release induced by hypertonic saline infusion was significantly increased 0.24 (0.15) pg/ml P[AVP]/mOsmol POsm, P< 0.05 compared to schizophrenia patients 0.07 (0.07) pg/ml P[AVP]/mOsmol POsm, in whom same response was abnormally low. Slopes for healthy control were 0.11 (0.09) pg/ml P[AVP]/mOsmol POsm, and not different than either group. These findings are consistent with implicated NMDA receptor related abnormalities in depression and schizophrenia in subgroups of patients, and provide the first in vivo evidence towards this dichotomy.