An American Woman Died From an Antibiotic-Resistant Infection
Are we seeing the end of the age of antibiotics?
When you get sick, you take medicine. If the medicine doesn’t help you get better, you try a different one. But what if you try 26 different drugs and none of them help? That scenario may sound far-fetched, but according to a Centers for Disease Control and Prevention report released on January 13, a woman died from Klebsiella pneumoniae, a strain of bacteria that was resistant to all 26 antibiotics approved for use in the United States. Deaths like this are becoming more likely as scientists predict that drug-resistant superbugs could kill 10 million people by 2050.
In the report, researchers at the CDC documented the case of a Nevada woman who died in an acute care hospital from an antibiotic-resistant bacterial infection. Scientists say that the 70-year-old likely died from a hip fracture that became infected, possibly during a recent hospital stay in India. Her death is cause for concern in and of itself, but what’s even more alarming is what doctors found after the patient died. In this case, doctors didn’t treat the patient with all 26 antibiotics that are available in America, but they treated her with multiple last-resort drugs, to no avail. They tested the bacteria, a carbapenem-resistant Enterobacteriaceae, after she died, and found that it was indeed resistant to all 26 antibiotics available in America. The bacteria was somewhat susceptible to the drug fosfomycin, but it’s not approved for intravenous use in the United States.
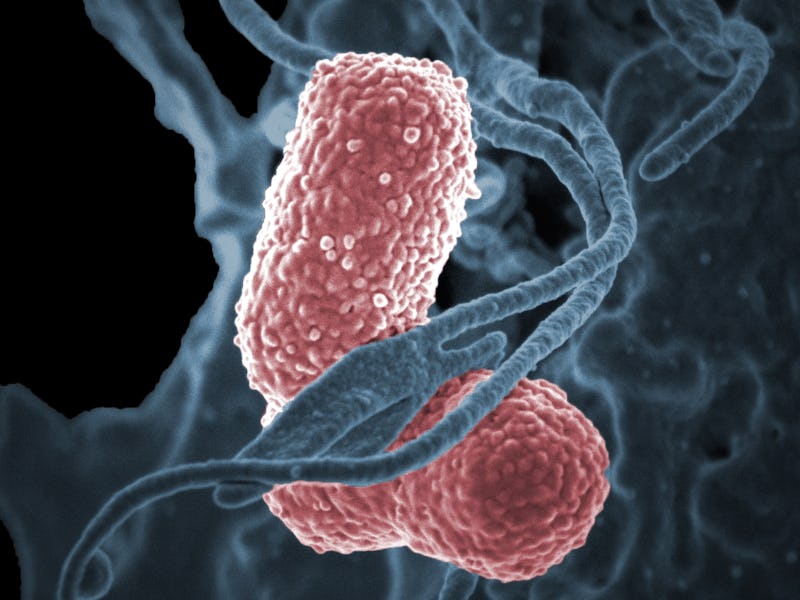
*Klebsiella pneumoniae* is a bacterium that causes serious infections in hospitals and can't be controlled with typical antibiotics
This problem is not new, and it’s getting worse. The rising tide of superbugs can be attributed in large part to the overuse of antibiotics, especially in livestock. Since bacteria are so good at exchanging genetic material, just one resistant individual can give its gift to many of its siblings in, say, the stomach of a pig.
But few farmers or ranchers have stepped up to change their habits, since thin profit margins can make scaling back the use of antibiotics a risky proposition. Besides, if the entire industry is using antibiotics to help control infections in herds, what incentive is there for any individual to stop? “We definitely need to have a much greater sense of accountability in terms of antibiotic resistance,” Timothy Walsh, an infection and immunity expert at Cardiff University, told Inverse back in 2015. Unfortunately, the situation has not improved much since then. And with new antibiotics being rendered useless in less time than it takes to develop them, we may be seeing the beginning of the end of the age of antibiotics.