Replicating Charlie Sheen's HIV Drug Success Will Cost a Fortune
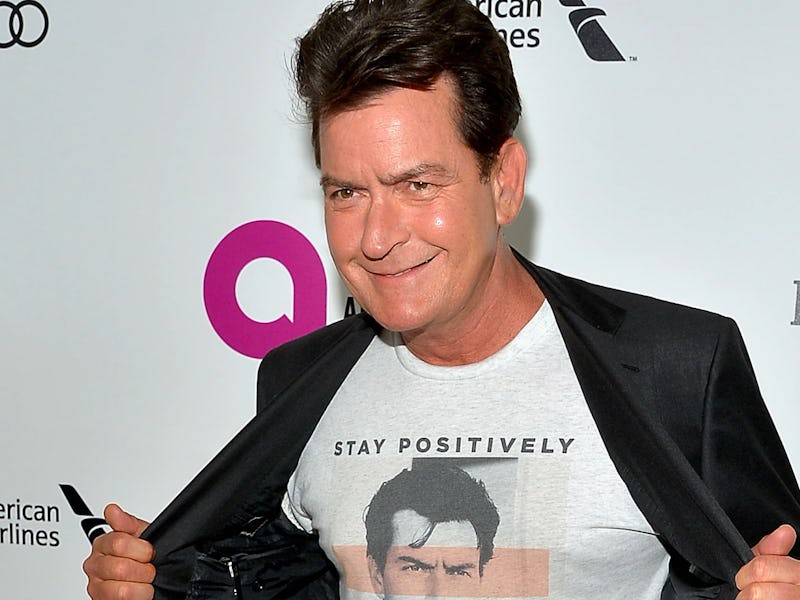
Last November, Charlie Sheen revealed that he was HIV positive. In July, his doctor announced that his patient was doing “phenomenal,” and in October Sheen said that he was part of an FDA-funded trial on an anti-HIV drug called PRO 140. Sheen’s experimental treatment appeared to be very successful: On Friday, he announced that his HIV has been fully suppressed. Replicating that success, unfortunately, probably won’t come cheap.
“Personally, I think about how I felt on the day and how I feel today,” Sheen told the Daily Mail Online. “I thought for sure I’d be stuck on that cocktail forever, but look at me now. I’m so grateful for the geniuses at CytoDyn for developing this and finding me.”
Sheen isn’t exactly cured — HIV is a virus that the human body can’t get rid of completely — but if the results are true, it does mean that his body is in a state where the immune system is able to fight off infections.
For treatment, Sheen has received weekly injections of PRO 140, which makes it different than highly active antiretroviral terapy (HAART), which is currently the standard of care for HIV. HAART is a combination of different classes of medications customized on the basis of the patient’s viral load, which is the amount of HIV in a sample of blood. The higher the viral load, the more HIV in the body.
HAART is what changed HIV/AIDS from being a fatal diagnosis to a manageable disease, but the creators of PRO 140 think they can do better. The drug comes from CytoDyn, a biotechnology company that announced in a press release in November that in each of its seven clinical trials, the drug has significantly reduced or controlled the HIV viral load in humans. So far, none of the trials have resulted in negative effects to the patient’s immune functions.
CytoDyn says that PRO 140 has been designated a “fast track” product candidate by the FDA and has received a National Institutes of Health grant of about $28 million.
However, the viral-entry inhibitor is also likely to be very, very expensive. That shouldn’t come as a surprise: The lifetime cost of treating HIV with antiretroviral drugs is estimated to be about $379,000. Taking four drugs a day that can individually cost between $200 and $3,000 dollars adds up. And according to the CDC, fewer than one in five people living with HIV has private insurance, while 30 percent have no coverage.
The Affordable Care Act has done a lot to allow people with HIV/AIDS to afford treatment, but the future of that legislation is uncertain. And according to CytoDyn’s investor presentation, it certainly doesn’t look like it’s going to be given out at a low price — at least, not in the immediate future. One of the company’s “investment highlights” is a note that the U.S. market size of HIV therapies is $15 billion.
What PRO 140 seems to be able to do is an incredible feat of science. Hopefully, the costs will allow it to actually help the millions of people who need it.